What is Conjunctiva? Today’s topic is all about the conjunctiva of the eye: definition, anatomy, layers, types, and function.
What is Conjunctiva of the Eye?
The conjunctiva of the eye is a thin, vascularized, semitransparent mucus membrane that covers the part of the anterior surface of the eyeball and the posterior region of the eyelids.
It is defined as an important eyeball covering that can’t be seen easily.
The clear tissue covers the sclera (white part of the eye) and becomes continuous with the corneal epithelium in the eyeball.
Similarly, the conjunctival tissue in the eyelid region gets merged with the skin at the lid margin.
Conjunctiva pronunciation
How to pronounce conjunctiva? The word conjunctiva is pronounced as kon·juhngk·tai·vuh in both American and British English.
The Latin term “conjoin”, which means “to join”, gave rise to the English word “conjunctiva”.
The Function of Conjunctiva
The conjunctiva tissue serves the following main functions in the eye.
-Produce mucus and tear to maintain the lubrication and keep the anterior surface of the eyeball moist.
The tear produced by the conjunctival tissue is negligible compared to that produced by lacrimal glands.
-Prevent eye irritation by reducing friction between eyelid and eyeball. The conjunctival sheet helps to maintain lubrication between the eyelid and eyeball during the closing and opening of the eyelid.
-Also helps to maintain the aseptic environment in the eye by preventing entry of pathogenic microbes, bust, dirt, and debris into the eye.
-Micro-blood vasculatures provide nutrients to the eyeball and eyelid tissues.
-The conjunctival sheath of the eye helps to maintain the tear film stability. Hence, help to prevent dry eye syndrome.
How conjunctiva of the eye combats infection
The conjunctiva of the eye fights infection and maintains an aseptic environment because of the following characteristic features of the conjunctival tissues.
-Conjunctiva is a highly vascular tissue
-Different types of defensive cells are present in the conjunctiva that can initiate and participate in defensive inflammatory reactions
-Immunocompetent cells are present in the conjunctiva that can contribute to the rich supply of immunoglobulins
-The foreign particles, such as a virus can be easily engulfed and neutralized by microvilli and enzymatic activities present in the conjunctiva
Microanatomy and Histology of the Conjunctiva of the Eye
Histologically, there are three layers of the conjunctiva. These three layers of the conjunctival tissue of the eye are the epithelium, adenoid layer, and fibrous layer.

Epithelium
The thickness and layers of the conjunctival epithelium vary in different types of the conjunctiva.
The marginal conjunctival sheet consists of 5 layers of non-keratinized stratified squamous epithelium.
Here, the superficial layer is composed of squamous cells, the intermediate layers are made up of polyhedral cells, and the deepest layer of the marginal epithelium is formed by the cylindrical cells.
The tarsal conjunctiva in the upper eyelid is double layered while the tarsal conjunctiva in the lower eyelid is composed of 3-4 layers of cells.
The superficial layer of the upper tarsal conjunctiva has cylindrical cells and the deep layer has cubical cells.
Similarly, in the lower tarsal conjunctiva, deep to superficial layers are made of cubical cells, polygonal cells, elongated wedge-shaped cells, and cone-shaped cells.
Conjunctival fornix and bulbar conjunctiva have three-layered epithelium.
Here, the superficial layer has cylindrical cells, the middle layer is composed of polyhedral cells, and the deep layer is made up of cuboidal cells.
The limbal conjunctival area has the largest number of epithelium layers compared to other types of the conjunctiva.
It has 8-10 layers of stratified squamous epithelium. Limbal conjunctiva contains papillae (palisades of Vogt).
The epithelium of the palisade zone provides a germinative zone for the corneal epithelium.
Adenoid layer
The adenoid layer or lymphoid layer is made of fine connective tissue reticulum containing lymphocytes.
Conjunctival fornices have the most developed adenoid layer. This layer is not present in newborn babies and develops at 2-3 months of life.
Hence, the conjunctival inflammation in an infant does not show follicles or follicular reactions.
Fibrous layer
The network of collagenous and elastic fibers gives rise to the fibrous layer of the conjunctiva. The thickness of the fibrous layer varies from region to region.
It is thinnest in the tarsal conjunctiva. Conjunctival blood vessels and nerves are found in the fibrous layer. In bulbar conjunctiva, this layer blends with the Tenon’s capsule.
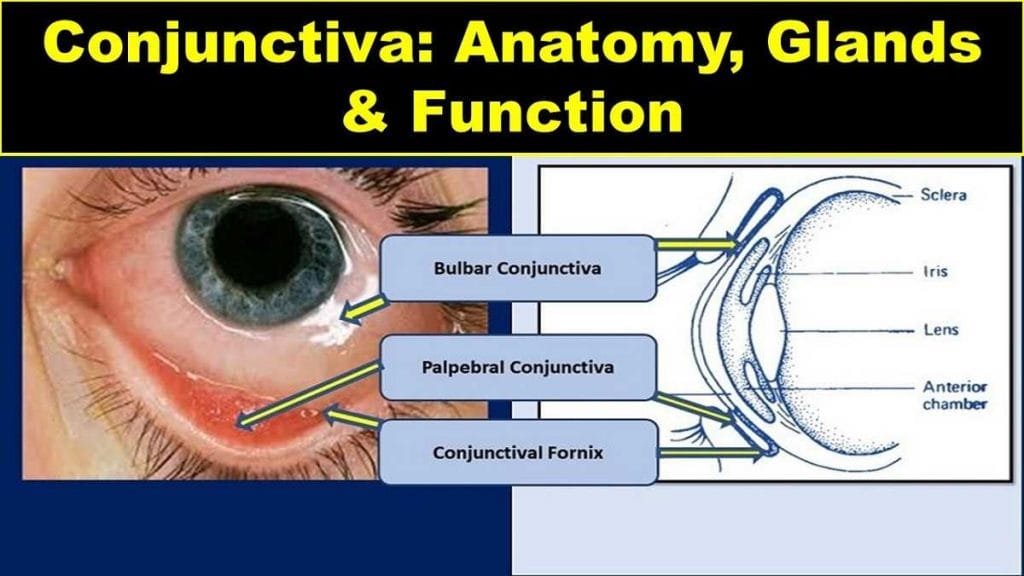
Types of Conjunctiva of the Eye
Conjunctiva is broadly divided into three parts or segments: palpebral conjunctiva, bulbar conjunctiva, and conjunctival fornix.
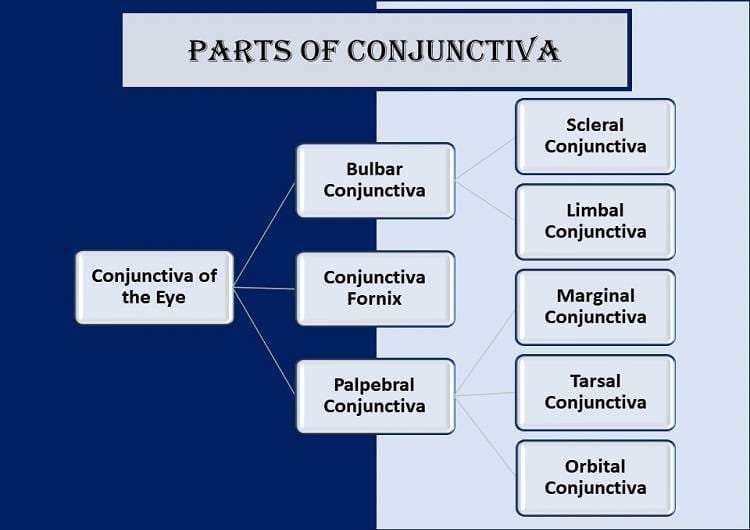
Palpebral Conjunctiva
The Palpebral conjunctiva is thick, opaque, highly vascular, and covered with numerous papillae, its deeper part presenting a considerable amount of lymphoid tissue.
Depending on the position of the eyelids, there are upper and lower palpebral conjunctiva.
The palpebral conjunctival tissue is subdivided into 3 parts: marginal palpebral conjunctiva, tarsal palpebral conjunctiva, and orbital palpebral conjunctiva (orbital zones).
Bulbar Conjunctiva
The bulbar conjunctiva is the thinnest of all the conjunctiva. It is so translucent that the underlying white part of the eye (sclera) and blood vessels are observed vividly.
Bulbar conjunctiva can be moved easily as it is loosely attached over the underlying episcleral tissues (except at the limbus and near insertions of the recti muscles).
In the episcleral region lie the anterior ciliary arteries, forming a pericorneal plexus, and tendons of the recti.
There are two parts of the bulbar conjunctiva: scleral conjunctiva and limbal conjunctiva.
The palpebral and bulbar conjunctiva form a continuous sheet between eyelid and eyeball.
It means the conjunctival sheet doesn’t allow any objects from the anterior region to pass towards the posterior covering of the eyeball.
Thus, it reduces the risk of anything gets lost behind the eye. It is useful clinically for contact lens wearers and prosthetic eye users.
Conjunctival Sac
Bulbar and palpebral conjunctiva and fornix form a sac in between eyelid and eyeball that opens at the palpebral fissure.
The conjunctival sac has the capacity to hold fluid up to 30 µl (microliter). The sac already contains about 7 µl of tear fluid forming a tear prism.
This knowledge is helpful to answer the query regarding how many drops of medicinal eyedrop can a person put in an eye at a time.
A standard eyedropper dispenses 0.05 ml (50 µl) per drop, meaning there are 20 drops per ml.
Based on this calculation we can say that one drop of eyedrop is more than enough for the eye to hold.
So, it is a complete waste of eyedrop if you use more than one drop at a time.
Conjunctival Fornix of eye
Conjunctival fornix or forniceal conjunctiva is a circular cul-de-sac that joins the palpebral and bulbar conjunctiva.
It is a continuous sheet that ends only on the medial or nasal side by the caruncle and the plica semilunaris.
The conjunctival fornix is comparatively thicker and loosely adhered to allow free eyeball movement.
Forniceal conjunctiva can be subdivided into superior, medial, inferior, and lateral fornix of the eye.
Plica Semilunaris
The plica semilunaris is a narrow crescentic fold of conjunctival fornix, concave laterally, and present in the medial canthus lying lateral to and partly behind the caruncle.
It is a vestigial structure in human beings. Plica semilunaris represents the nictitating membrane of the lower animals.
The plica reaches the middle of the lower fornix below and extends less far above. 2 mm recess separates the free lateral border from the bulbar conjunctiva, and it disappears in the lateral gaze of the eyeball.
Its vascular, pink color contrasts with the white part of the eye, the sclera.
Caruncle
The caruncle (Latin caro=flesh) is a small, soft, pinkish mass in the inner or nasal canthus medial to the plica semilunaris.
It is a piece of modified skin and has sweat glands, hair follicles, and sebaceous glands.
The caruncle is about 5 mm high and 3 mm broad. It adheres to the plica semilunaris, and fibers of the medial rectus sheath.
Hence, the caruncle is prominently visible in lateral gaze and becomes retracted on the medial gaze of the eyeball.
Conjunctival Glands
Two types of glands that are present in the conjunctiva are the mucin secretory glands and the accessory lacrimal glands.
Mucin secretory glands are crypts of Henle, glands of Manz, and the goblet cells.
Among these mucin secretory glands, goblet cells are the unicellular glands present within the conjunctival epithelium, crypts of Henle are located in the tarsal conjunctiva and the glands of Manz are present in the limbal conjunctiva.
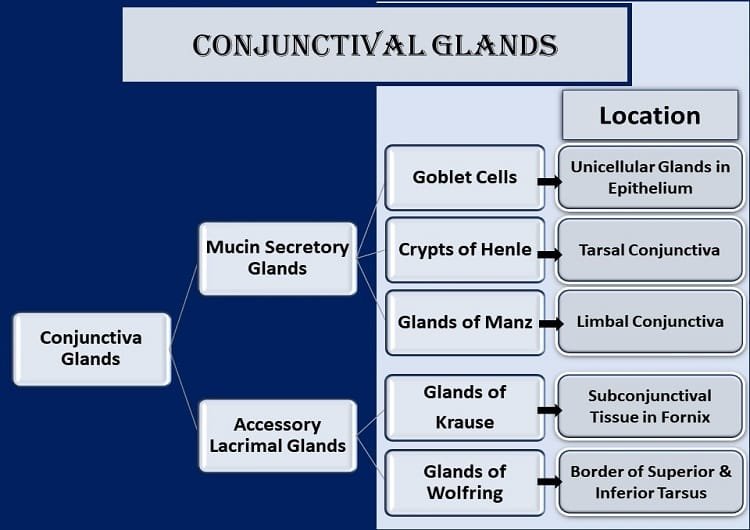
Glands of Krause and glands of Wolfring are known as the accessory lacrimal glands. Glands of Krause are found in the subconjunctival connective tissue of the fornix.
There are about 6-8 glands in the lower conjunctival fornix and 42 in the upper fornix. Likewise, glands of Wolfring are located along the upper border of the superior tarsus and the lower border of the inferior tarsus.
There are around 2-5 glands in the upper tarsus and 2 glands in the lower border of the inferior tarsus.
Blood Supply to the Conjunctiva of the Eye
Different parts of the conjunctiva are supplied by the arteries derived from these three sources:
- Anterior Ciliary arteries
- Marginal arcade of the eyelid
- Peripheral arcade of the eyelid
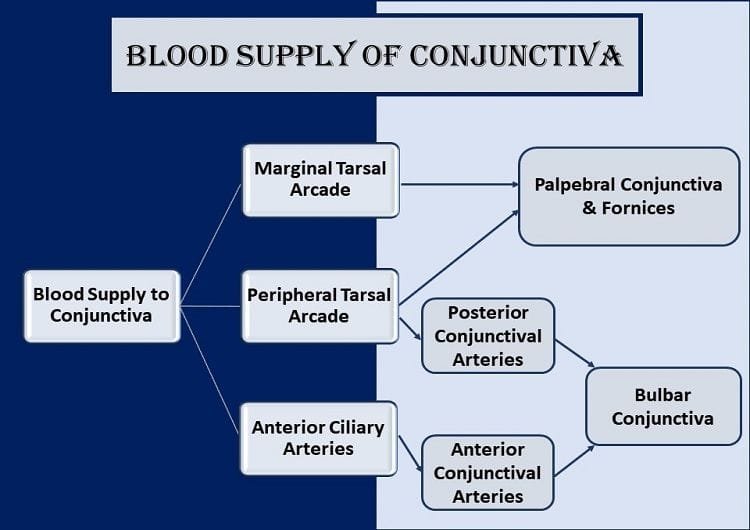
Arterial branches from the marginal and peripheral arcade of eyelids supply blood to the conjunctival fornices and palpebral conjunctiva.
Bulbar conjunctiva gets blood supply from two sources: anterior conjunctival arteries and posterior conjunctival arteries.
The anterior conjunctival arteries are the branches of anterior ciliary arteries and the posterior conjunctival arteries derive from the arterial arcades of the eyelids.
The anastomosis of these two types of arteries gives rise to pericorneal plexus.
The veins around the cornea drain blood from the conjunctival tissues into the anterior ciliary veins and veins from the remaining parts of the conjunctiva drain blood into the venous plexus of the eyelids, and ultimately to the superior and inferior ophthalmic veins.
Lymphatic Drainage
The lymphatic drainage of the different parts of the conjunctiva is done via lymphatics of eyelids, preauricular lymph nodes, and submandibular lymph nodes.
Lymphatics in the palpebral conjunctiva drain their contents into the lymphatics of the underlying eyelids.
Similarly, medial or nasal bulbar conjunctival lymphatics drain into the submandibular lymph nodes whereas the lateral or temporal bulbar conjunctival lymphatics drain their contents into the preauricular lymph nodes.

Nerve Supply to Conjunctiva of Eye
Conjunctival nerve innervation is done by the ophthalmic division (first division) of the trigeminal nerve.
Majority of the nerve fibers that supply the conjunctiva lose their myelin sheaths and form a subepithelial plexus in the superficial substantia propria.
The nerve fibers then form an intraepithelial plexus around the bases of the epithelial cells, sending free fibrils between them.
The same nerves supply both eye eyelids and the majority of the conjunctiva. But, the limbal conjunctiva in the circumcorneal zone is innervated by the long ciliary nerves.
Likewise, the lacrimal nerve, the supraorbital and supratrochlear nerves, infraorbital and infratrochlear nerves supply the vast majority of the conjunctiva.
The nerve endings are either naked, free, or with end bulbs.
Clinical Significance of Conjunctival Tissue
Being exposed to the outer environment, conjunctiva poses varieties of ocular complaints. It is also an important ocular tissue upon examination of which we can get an idea of many systemic illnesses.
So, there are several clinical significances of the conjunctiva of the eye.
- diabetes alters the micro blood vessels of the conjunctiva. It is useful to diagnose and monitor the stages of diabetic retinopathy by just examining the changes in the bulbar conjunctival blood vessels.
- increased tortuosity of blood vessels and capillaries in the bulbar conjunctiva suspects systemic hypertension, and hence hypertensive retinopathy.
- slower blood flow in conjunctival blood vessels might be the sign of carotid artery occlusion.
- altered blood flow and blood vessel diameter might be due to sickle-cell anemia
- tumors seen in conjunctiva may indicate tumors in other parts of the body (mostly in the malignant tumor).
Conjunctival Disorders
Inflammation of conjunctiva (conjunctivitis)
The inflammation of the conjunctival tissue is termed “conjunctivitis”. Also known as pink eye, conjunctivitis is the most common cause of red-eye.
The common symptoms of conjunctivitis include redness, stickiness, grittiness (foreign body sensation), watering, burning sensation, dryness, and itchiness.
Pain, blurry vision, and photophobia should be given extra attention in inflammation of the conjunctiva as they are not typical characteristics of a primary conjunctival inflammatory response.
These features suggest underlying ocular or orbital disease processes including keratitis, uveitis, acute glaucoma, and orbital cellulitis.
Degenerative Conditions of the Conjunctiva of the Eye
The common conjunctival degenerations are pinguecula, pterygium, and concretions.
Pinguecula
Pinguecula is a yellowish-white fleshy patch on the bulbar conjunctiva near the conjunctiva-cornea junction (limbus).
Several predisposing factors such as aging, exposure to strong sunlight, dust leads to degeneration of the substantia propria of the conjunctiva.
As a consequence, the pinguecula is formed.
As a matter of fact, pinguecula most commonly affects the nasal bulbar conjunctiva first. The apex of any pinguecula is always away from the cornea. It is also considered the precursor of pterygium.
Pterygium
Pterygium is a wing-shaped fold of degenerated conjunctival tissue which encroaches upon the cornea.
It destroys the corneal epithelium layer, bowman’s layer, and superficial corneal stroma. Grittiness or foreign body sensation, blurry vision (in advanced pterygium), and diplopia (rarely) are the symptoms of pterygium.
Concretion
Sometimes, small, yellowish-white deposits are seen in the palpebral region. It is concretion. The compositions of the concretion are epithelial inclusion cysts filled with epithelial and keratin debris.
Concretions rarely give a symptom of foreign body sensation. Usually, they are asymptomatic.
Conjunctival Tumors
There are two types of tumors in the conjunctiva, malignant or benign, based on the tissue of origin.
Papilloma and squamous cell carcinoma are benign and malignant tumors at the epithelial surface respectively.
An adenoma is a benign tumor in glandular tissue while adenocarcinoma is a malignant tumor.
In connective tissue, fibroma is a benign tumor and sarcoma is a malignant tumor. Likewise, hemangioma is a benign tumor of vascular tissue when angiosarcoma is the malignant one.
A benign tumor in the reticular system is called lymphoid hyperplasia, and a malignant tumor is known as lymphosarcoma.
Similarly, naevus is a benign tumor in pigment cells while melanoma is a malignant tumor.
YOU MAY ALSO LIKE
Colored Part of the Eye: Iris Definition, Function, & Anatomy
Blurry Vision In The Morning – Causes And Concerns
Wavy Squiggly Lines in Vision (Eye Floaters)
Bulbar Conjunctiva, Palpebral Conjunctiva, and Fornix of Eye
White Part of the Eye: Sclera Function, Definition & Anatomy
What is Cornea of Eye: Function, Definition, Anatomy, Layers
Cranial Nerves Mnemonic: How to Memorize Fast
References
- Wolff’s Anatomy of the Eye and Orbit by Anthony J. Bron, Ramesh C. Tripathi, Brenda J. Tripathi
- Comprehensive Ophthalmology Fourth Edition by A. K. Khurana