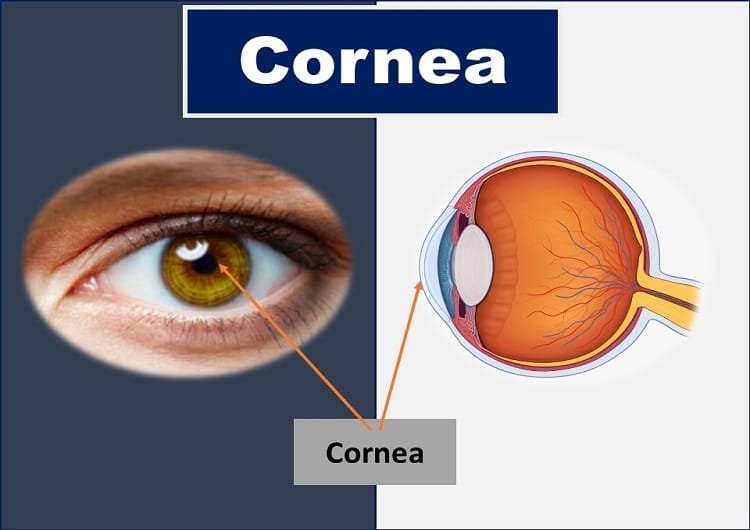
All about Cornea of the Eye: Definition, Function, Anatomy, Blood Supply, & Nerve Supply of the Cornea of Eye.
Cornea Definition
What is the cornea of the eye? The cornea is defined as the transparent, avascular, dome-shaped, or watch-glass-like window of the front of the eye. It is the most anterior one-sixth of the fibrous, protective coat or covering of the eyeball.
The cornea covers the important eye structures such as the pupil (the circular opening at the center of the iris), iris (the structure that gives color to the eye), anterior chamber (fluid-filled between iris and posterior surface of the cornea), and the crystalline lens (light focusing and accommodating structure of the eye).
From an optical perspective, the cornea is the most vital refractive organ of the eye. In humans, it has approximately three-fourths (43 dioptres) of the total refractive power (60 dioptres) of the eye.
The light entering the eye gets refracted by the cornea, and passes through the pupil, lens, and vitreous before focusing on the retina to form a real, inverted image of any object.
The refractive surgeries or laser surgeries that are done to correct refractive errors (LASIK, LASEK, and more) are mainly the corneas reshaping surgical procedures.
Likewise, contact lenses of any type that are prescribed for clear vision, comfort, cosmesis, and therapeutic purposes are worn over the corneas.
The medical term “cornea” is derived from the Greek word “κέρας, that is kertato” which means horn or shield-like. Hence, almost all medical terms related to the cornea often start with the prefix “kerat-”.
Embryology or Development of Cornea
Corneal embryogenesis involves multistep processes. The cellular interactions between the tissues of ectodermal origin give rise to various layers and parts of the cornea of the eye that are summarized below.
- The presumptive corneal epithelium is derived from the bilateral interactions between the cranial ectoderm and the neural ectoderm-derived optic vesicles.
- The endothelium, Descemet’s membrane, and the stromal keratocytes are formed by the migration of the neural crest cells in between the lens and presumptive corneal epithelium. The interaction of the neural tube with the adjacent ectoderm forms a neural crest.
- The sensory nerves originate from the trigeminal ganglion which is derived from the neural crest and the ectodermal placode. The sensory nerves supply the epithelium and corneal stroma.
Dimensions of Cornea
The front surface or the anterior surface of the cornea is elliptical due to the greater overlap of the sclera and conjunctiva above and below the cornea. The average horizontal diameter at the front is 11.7 mm, and the average vertical diameter is 10.6 mm.
Similarly, the back or posterior surface of the cornea of the eye is circular with an average diameter of about 11.7 mm. According to Priestly-Smith (1890), the cornea is 1% wider in men than in women.
Microcornea is a condition where the anterior corneal surface diameter is less than 10 mm. Likewise, macrocornea has an anterior corneal diameter of more than 13 mm.
The axial or the central thickness of the cornea of the eye is about 0.52 mm (Donaldson, 1966; Maurice, 1969) whereas the paraxial or the peripheral thickness is 0.7 mm.
According to Smelser (1960), the cornea in a newly born is slightly thicker than that in children. It reflects the endothelial function and loss that starts from birth. The surface area of the cornea is about 1.3 cm2, one-sixth of the total surface area of the eyeball.
The central 5 mm area of the cornea is an optically crucial structure as it is the most important refracting surface of the eye for image formation.
Topographically, the anterior and the posterior radii of curvature of the central 5 mm area of the cornea are 7.8 mm and 6.5 mm, respectively.
This difference in horizontal and vertical radii of curvature gives rise to astigmatism of some amount even in emmetropes.
As we already mentioned, the cornea is the most powerful refractive surface of the eye. It has roughly three-fourth (45 dioptres) of the total refractive power of the eye (60 dioptres)
Functions of Cornea of the Eye
The anatomical function of the eye cornea is to protect the inner ocular structures and maintain the shape of the eyeball. Along with the sclera, conjunctiva, and tear film, the cornea helps to shield the inner eye tissues from germs, dust, and other harmful matter.
The cornea of the eye plays a pivotal role in the optical functioning of the eye. So, it is also known as the window to the eye.
Being the transparent eye structure, the cornea allows almost all light rays to pass through it, which forms the basis of image formation on the retina. It contributes between 65- 75 percent of the eye’s total focusing power.
The optical role of the cornea is crucial in the sense that even the slightest change in the corneal surface and layers leads to refractive errors such as myopia, hypermetropia, and astigmatism.
In general, flattening of the curvature of the cornea results in hyperopia, the steepening of the surface gives rise to myopia and uneven changes or irregularity in the corneal surface results in astigmatism.
When light rays enter the cornea, it bends or refracts the incoming light onto the lens. The lens further refocuses or accommodates that light onto the retina, a layer of light-sensing cells lining the back of the eye that starts the translation of light into vision.
To see clearly, light rays must be refracted by the cornea and accommodates by the lens to fall precisely on the retina. The retina converts the light rays into neural impulses that are sent through the optic nerve to the brain, which interprets them as images.
The image formed on the retina is inverted, that is made erect by the visual processing on the brain.
The refractive process that takes place in the eye is similar to the way a camera takes a picture. The cornea and lens in the eye act as the camera lens. The retina is similar to the camera film. If the image is not focused properly, the film (or retina) receives a blurry or defocused image.
The cornea also serves as a protective filter, cutting out some of the most damaging ultraviolet (UV) wavelengths in sunlight. Without this protection, the lens and the retina would be highly susceptible to injury from UV radiation.
Along with the above-mentioned functions of the overall cornea, the individual layers have some specialized functions as below.
Epithelium
Corneal epithelium provides a smooth surface for the tear film to spread uniformly across the surface of the eye. Tear film helps to keep the eye surface moist, prevents dryness, maintains eye health and stable vision. Any deformity or irregularity on the epithelium degrades the quality of vision and eye health status.
Bowman’s Layer
The dense and stout Bowman’s layer prevents entry of most of the harmful microbes and reduces the risk of penetrating injuries. Once injured, this layer can’t be healed without a permanent scar, which can affect vision. Abrasion and injury to the epithelium heal quickly without any scarring.
Stroma
The stroma is metabolically the most significant layer of the cornea. Any injury and edema to the stroma leads to deteriorated vision and compromised eye health. Scratches and penetrating injury to the corneal stroma typically leave permanent scars that affect vision.
Endothelium
The endothelium is a single layer of cells. This layer acts as a barrier between the cornea and aqueous humor. It plays an important role to maintain fluid content in the cornea. Once destroyed, the cells can’t be regenerated and space will be occupied by the enlargement of the adjacent cells. The edema of the endothelium leads to reduced vision.
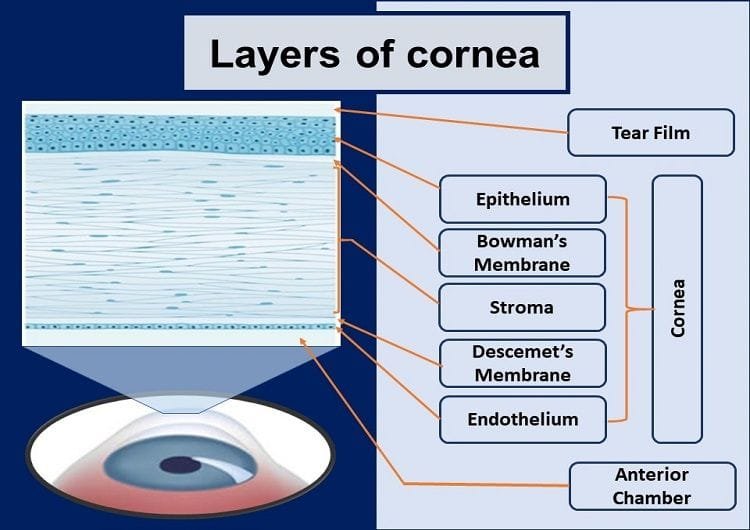
Histology of Cornea: Corneal Layers
There are five layers of corneal tissue behind the precorneal tear film. They are:
- Epithelium
- Bowman’s Layer
- Stroma
- Descemet’s membrane
- Endothelium
Epithelium
The corneal epithelium is of nonkeratinized stratified squamous type and becomes continuous with the epithelium of bulbar conjunctiva at the limbus. The cells are held together by the desmosomes and to the basal lamina by the hemidesmosomes.
The epithelium has 5-6 layers of cells. The basal layer consists of columnar cells, the superficial 2 layers have flattened cells, and in between them, are 2-3 layers of wing or umbrella-shaped cells.
The superficial cells of the corneal epithelium play a vital role in tear film stability. These cells have microvilli and microplicae, and the cells secrete glycocalyx which helps in the adhesion and stability of tear over the cornea of the eye.
Bowman’s Layer
Below the corneal epithelium, there is a layer of acellular mass formed of condensed collagen fibrils, known as the Bowman’s membrane. This layer is named after English anatomist and ophthalmologist William Bowman.
The Bowman’s membrane is about 12 µm in thickness. Because of the compact arrangement of collagen fibers, it is comparatively resistant to infection and trauma and binds the corneal stroma anteriorly with the basement membrane of the epithelium. Bowman’s membrane once destroyed, can’t get regenerated.
Stroma
The stroma or the substantia propria constitutes most of the cornea. It is about 0.5 mm thick and makes up 90% of total corneal thickness.
The stroma consists of collagen fibrils, keratocytes, and extracellular ground substances. The multilayered lamellae are arranged parallelly to each other and to the plane of the cornea.
The mean diameter of individual collagen fibers and mean distance between collagen fibers are almost equal and both of them are less than half of the wavelength of light (400-700nm).
As a consequence, the scattering of incident light by a collagen fiber is neutralized or canceled by destructive interference. This arrangement of collagen fibers helps to maintain corneal transparency. The lamellae become continuous with scleral lamellae at the limbus.
The ground substances present among the lamellae consist of keratocytes, histiocytes, wandering macrophages, and a few leucocytes. Keratin sulfate and chondroitin sulfate are major glycosaminoglycans of the stroma.
Descemet’s Membrane
The Descemet’s membrane or the posterior elastic lamina bounds the stroma posteriorly. It is a thick basement membrane or a strong homogenous layer secreted by the endothelium. Descemet’s membrane is made of collagen and glycoproteins, and it is highly resistant to trauma, chemicals, and pathogens.
The thickness of the Descemet’s membrane varies according to the age of the person. It is about 3 µm thick at birth, 10 µm in adults, and thickens with age. It terminates near the limbus at the anterior limit of trabecular meshwork as Schwalbe’s lin.
The Descemet’s membrane doesn’t consist of any elastic fibers and the elastic property is achieved due to the peculiar arrangement of collagen fibers. This layer of the cornea is always in a state of tension and when torn it curls inwards on itself.
Endothelium
Behind the Descemet’s membrane is a single layer of about µm thickness consisting of flat hexagonal cells, known as the endothelium. The cells appear as a continuous mosaic pattern in a slit lamp bio-microscopy. The endothelial cells are interconnected with each other by various junctional complexes like zonula occludans, macula occludans, and macula adherens. These cells possess the ion transport system or active pump mechanism which is known as an endothelial pump. These active pumps regulate the water content of corneal stroma.
The cell density of endothelium is around 3500 cells/mm2 in newborns, 2500 cells/mm2 in young adults, which decreases with the advancing age as these cells can’t divide or regenerate. There is a considerable functional reserve for the endothelium. Therefore, corneal decompensation occurs only after more than 75 percent of the cells are lost.
The two popular cell mechanisms occur in the endothelium of the cornea: Polymegathism and pleomorphism. Polymegathism is the increase in cell size and pleomorphism is a change in cell shape in order to compensate for the reducing cell density with age in the corneal endothelium layer.
Nerve Supply of the Cornea of Eye
The anterior ciliary nerves supply the cornea. These nerves are branches of the ophthalmic division of the trigeminal nerve (5th cranial nerve). The nerves lose myelination after penetrating the cornea and forms three corneal plexuses. The stromal, subepithelial, and intraepithelial plexuses supply the respective layers of the cornea.
The cornea has a high density of nerve endings. Because of this, the cornea is one of the highly sensitive tissues in the body. It is found that the cornea is around 300 times more sensitive than the body skin. There are as many as 100 nerve endings in an area of 0.01 mm2.
In corneal pathology, patients may experience severe pain due to exposure of the nerve endings. Likewise, the reduced corneal sensitivity might indicate damage to the corneal nerve endings by herpes simplex viral infection.
Blood Supply to the Cornea of Eye
In normal conditions, the cornea is devoid of blood vessels. The avascular nature contributes to maintaining corneal transparency. Small vessels from the anterior ciliary artery, which is the branch of the ophthalmic artery invade the subconjunctival tissue over the cornea in the peripheral region. This vascular arcade in the peripheral cornea (in the limbal region) helps in corneal metabolism and wound healing by providing essential nutrients.
The hypoxic, infectious, or allergic conditions trigger corneal vascularization (growth of fine blood vessels onto the clear corneal surface) to supply more oxygen and nutrition to the affected cornea. These fine vessels stop carrying blood to the cornea after the restoration of normal corneal condition. However, the vessel outlines are still visible as ghost vessels. For instance, in the corneal pannus, there will be the growth of fine blood vessels onto the clear corneal surface (mostly onto the superior corneal region). An ill-fitted contact lens is the common cause of pannus formation.
YOU MAY ALSO LIKE
Colored Part of the Eye: Iris Definition, Function, & Anatomy
Diplopia Charting: Common Method of Double Vision Test
Hess Charting: Interpretation of Hess Screen Test
Blurry Vision In The Morning – Causes And Concerns
Wavy Squiggly Lines in Vision (Eye Floaters)
Bulbar Conjunctiva, Palpebral Conjunctiva, and Fornix of Eye
What is Conjunctiva of the Eye?
White Part of the Eye: Sclera Definition, Function, and Anatomy
Cranial Nerves Mnemonic: How to Memorize Fast
Right & Left Eye Twitching Meaning
Sudden Blurry Vision in One Eye: Causes, and Treatment
References
- Wolff’s Anatomy of the Eye and Orbit by Anthony J. Bron, Ramesh C. Tripathi, Brenda J. Tripathi
- Comprehensive Ophthalmology Fourth Edition by A. K. Khurana