All About Dots in Eyes & Spots in Eyes (Ophthalmology): Gunn’s dots, Roth’s spot, Koplik’s spots, Bitot’s spot, Fuchs’ spot, and many more.
Dots in Eyes & Spots in Eyes (Ophthalmology) gives you a comprehensive list of all the important dots and spots observed in all structures of the eye; from the anterior-most cornea to the posterior retina. This important list of spots and dots in the eyes is equally useful for medical students, medical practitioners, paramedics, nurses, and researchers in the field of medicine.
The list can be a good companion for medical students preparing for any type of entrance exams and university exams. Dots in Eyes & Spots in Eyes (Ophthalmology) is a useful nursing guide for those who are participating in USMLE and other academic and professional exams. So, without further ado let’s jump into the topic.

Dots in Eyes(Dots in Ophthalmology)
Gunn’s Dots in Eyes (Ophthalmology)
Gunn’s dots are visible reflections of the internal limiting membrane, created by the footplate of the Muller cells. Robert Marcus Gunn originally described these reflections in 1918. Marcus Gunn used an ophthalmoscope based on a mirror and a solid flame as an illuminating source to observe them.
These tiny white specks are sometimes visible overlying the large vessels near the optic nerve or the nerve fiber layers. Their presence depends on lighting conditions, and they have no pathologic significance but some describe Gunn’s dot as a cause for photosensitivity.
Horner-Trantras Dots in Eyes (Ophthalmology)
Horner-Trantras dots are the hallmarks of vernal keratoconjunctivitis (VKC). In VKC, there is thickening and nodule formation of the conjunctiva near the limbus with the confluence of the nodules. The gelatinous dots on top of the nodules are Horner-Trantas dots consisting of desquamated epithelial cells. It is formed by the chalky collections of eosinophils at the limbus.
Kayes Dots in Ophthalmology (Eyes)
Kayes dots are white punctate subepithelial infiltrates located in the epithelium anterior to the suture line of a corneal graft. The dots (sometimes elevated line) represent epithelial cells in various stages of degeneration on histopathology and it has been hypothesized that they may result from an epithelial response to the area of tissue angulation. This is a sign of corneal graft rejection.
Mittendorf’s Dots in Ophthalmology (Eyes)
A Mittendorf dot is a small, whitish spot (on direct illumination) at the posterior lens surface (capsule), classically nasal in location. It represents the anterior attachment of the embryological remnant of the hyaloid artery. Failure of complete degeneration of embryonic particles can lead to benign findings, such as a Mittendorf dot or a Bergmeister’s papilla, or pathologic changes as seen in persistent fetal vasculature syndrome.
Mittendorf’s dot is associated with the posterior polar cataract. Care should be given during hydrodissection as there is a risk of posterior capsule (PC) rupture.
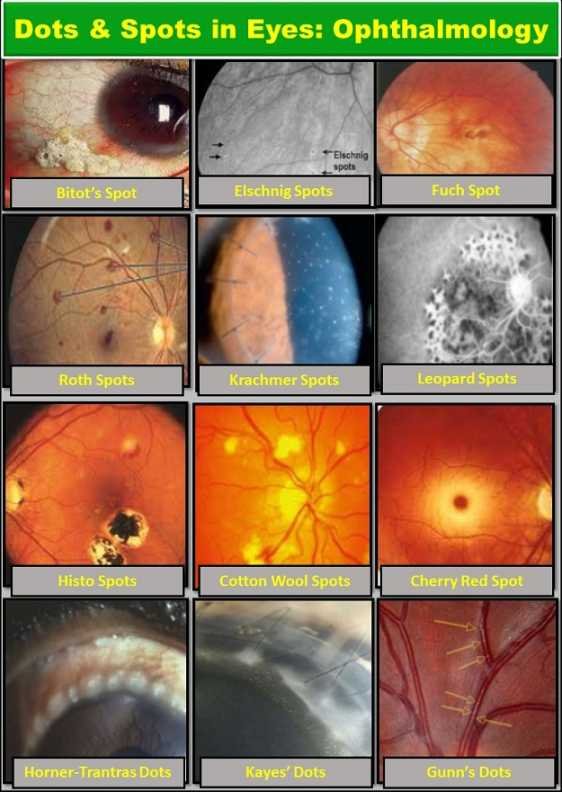
Spots in Eyes
Bitot’s Spots in Eyes (Ophthalmology)
Bitot’s spots are white, a foamy area located on the nasal and temporal conjunctiva. These are the buildup of keratin which is oval, triangular, or irregular in shape. Bitot’s spots are formed by the metaplasia of the conjunctival squamous cell of bulbar conjunctiva with the keratin layer.
Bitot’s spots are typically found in eyes of males and are a sign of vitamin A deficiency. In severe conditions, Bitot’s spots are associated with conjunctival xerosis, corneal xerosis, keratomalacia, corneal ulceration, and night blindness.
They have also been found in patients with normal or high levels of vitamin A with generalized malnutrition. Bitot’s spots may also occur secondary to gastrointestinal disease, alcoholic cirrhosis, hepatitis, bowel resections, abetalipoproteinemia, and cystic fibrosis. Pierre Bitot (1822-1888), a French physician, first described these spots in 1863.
High-dose vitamin A is the treatment for all individuals with xerophthalmia and for infants or children with severe malnutrition or measles. Improvement of Bitot’s spots is seen within 2 weeks of high-dose vitamin A therapy. However, the retinal manifestations of vitamin A deficiency are slower to respond to treatment, with night blindness and dark adaptation problems often persisting for 4 weeks.
Elschnig Spots in Ophthalmology (Eyes)
Elschnig’s spots are hyperpigmented patches in the choroid surrounded by a ring of hypopigmentation (black spots surrounded by bright yellow or red halos). These are seen on the retina with advanced hypertensive retinopathy. Choriocapillaris hypoperfusion gives rise to Elschnig spots. They got their name after Anton Elschnig.
Acute hypertensive changes of choroidal blood vessels are the major causes of Elschnig’s spots. The spots are commonly seen in young patients as their blood vessels are not ready to withstand the changes in blood pressure.
These changes in blood pressure cause an infarct of the vessels leading to the death of the retinal pigment epithelium (RPE) and photoreceptors they support creating this window defect.
Fuchs Spots in Eyes (Ophthalmology)
Also known as Forster-Fuchs’ retinal spot, the Fuchs spot is a degeneration of the macula in high myopia. It is named after the two persons who first described it: Ernst Fuchs, who described a pigmented lesion in 1901, and Forster, who described subretinal neovascularization in 1862.
The sizes of the spots are proportionate to the severity of pathological myopia. The first signs of a Fuchs spot are the distorted sight of straight lines near the fovea, which some days later turn to the typical well-circumscribed patches after absorption of hemorrhage, and a pigmented scar remains.
Brushfield Spots in Ophthalmology (Eyes)
Brushfield spots are small, white, or grayish/brown spots on the periphery of the iris in the human eye due to the aggregation of connective tissue, a normal iris element. The spots are named after the physician Thomas Brushfield, who first described them in his 1924 M.D. thesis.
These spots are normal in children (Kunkmann-Wolffian bodies) but are also a feature of the chromosomal disorder Down syndrome. They occur in 35–78% of newborn infants with Down syndrome.
They are much more likely to occur in children with Down syndrome of European descent than children of Asian heritage with Down’s Syndrome.
They are focal areas of stromal hyperplasia, surrounded by relative hypoplasia, and are more common in patients with lightly pigmented irises.
Roth’s Spots in Eyes (Ophthalmology)
Roth’s spots are retinal hemorrhages with white or pale centers. The original retinal spots identified in 1872 were attributed to nerve fibers that had burst or exploded.
The present-day analysis shows that they can be composed of coagulated fibrin including platelets, focal ischemia, inflammatory infiltrate, infectious organisms, or neoplastic cells. They are typically observed via fundoscopy (using an ophthalmoscope to view inside the eye) or slit lamp exam.
They are usually caused by immune complex-mediated vasculitis often resulting from bacterial endocarditis. Roth’s spots may be observed in leukemia, diabetes, subacute bacterial endocarditis, pernicious anemia, ischemic events, hypertensive retinopathy, and rarely in HIV retinopathy. Roth’s spots are named after Moritz Roth.
Koplik’s Spots in Ophthalmology (Eyes)
Koplik spots (also Koplik’s sign) are a prodromic viral enanthem of measles manifesting two to three days before the measles rash itself.
They are characterized as clustered, white lesions on the buccal mucosa (opposite the lower 1st & 2nd molars), conjunctiva and are pathognomonic for measles.
The textbook description of Koplik spots is ulcerated mucosal lesions marked by necrosis, neutrophilic exudate, and neovascularization. They are described as appearing like “grains of salt on wet background“, and often fade as the maculopapular rash develops.
Fischer-Khunt Spots in Eyes (Ophthalmology)
Fischer-Khunt spot is seen as blue-grey plaque anterior to horizontal recti insertions. It appears in old age as Senile Scleral plaque and area of Hyalinised Sclera.
Krachmer Spots in Ophthalmology (Eyes)
In corneal graft, subepithelial rejection is characterized by subepithelial infiltrates, reminiscent of adenoviral infection (Krachmer spots) on the donor cornea, with deeper edema and infiltrative opacification.
Stromal rejection features a deeper haze. It can be chronic or hyperacute, the latter in association with endothelial rejection.
Leopard Spots in Eyes
Leopard spot appears as a patchy subretinal infiltrate in ocular conditions like reticular cell carcinoma, central serous chorioretinopathy (CSR), and other conditions of the retina.
Cherry Red Spots in Eyes (Ophthalmology)
A cherry-red spot is a finding in the macula of the eye in a variety of lipid storage disorders and in central retinal artery occlusion. It describes the appearance of a small circular choroid shape as seen through the fovea centralis.
The appearance of a cherry-red spot is due to the relative transparency of the macula. The storage disorders cause the accumulation of storage material within the cell layers of the retina. However, the macula, which is relatively devoid of cellular layers, does not build up this material, and thus allows the eye to see through the macula to the red choroid below.
The sign was first described by Warren Tay, a founding member of the British Ophthalmological Society, in 1881, with reference to a patient with Tay–Sachs disease.
The cherry-red spot is seen in central retinal artery occlusion, appearing several hours after the blockage of the retinal artery occurs.
Histo Spots in Ophthalmology (Eyes)
A histo spot is a small circular punched-out spot found in the retina at a site where spores of the fungus Histoplasma (histo) seeded in the eye. Histo spots may be multiple, found in both eyes, and scattered throughout the retina.
It is seen in presumed ocular histoplasmosis syndrome (POHS). Histo spots in the macula are significant since they may stimulate the growth of abnormal new blood vessels located under the retina.
These new blood vessels may suddenly bleed, causing permanent macular scarring and impairing central vision. If the process is detected at an early stage, it may be successfully treated with a focal retinal laser.
Cotton Wool Spots in Eyes (Ophthalmology)
Cotton wool spots appear as fluffy white patches on the retina. These are abnormal finding on the funduscopic exam of the retina of the eye. Cotton wool spots are caused by damage to nerve fibers and are a result of accumulations of axoplasmic material within the nerve fiber layer.
There is reduced axonal transport (and hence backlog and accumulation of intracellular products) within the nerves because of the ischemia. This then causes the nerve fibers to be damaged by swelling in the surface layer of the retina.
A 1981 analysis concluded that “in most instances, cotton-wool spots do not represent the whole area of the ischaemic inner retina but merely reflect the obstruction of axoplasmic flow in axons crossing into much larger ischaemic areas”.
Associated findings include microvascular infarcts and hemorrhages. The appearance of cotton wool spots may decrease over time. Abundant cotton wool spots are seen in Malignant hypertension.
Cream-Colored Spots in Ophthalmology (Eyes)
Cream-colored spots are the classic diagnostic features of birdshot vitiligenous chorioretinitis. These spots are as large as 0.5 to 1 disc diameter and are scattered throughout the fundus.
Sources
- Alexander, author, Larry J. (2002). Primary care of the posterior segment (3rd ed.). New York: McGraw-Hill, Medical Pub. Division. p. 331. ISBN 0-07-136476-5. [View]
- https://www.aao.org/eyenet/article/management-of-bitot-s-spots
- Sanez, R.B. (January 1999), “Primary care of infants and young children with Down syndrome”, American Family Physician, 59(2), p. 381
- Steichen O, Dautheville S (2009). “Koplik spots in early measles”. CMAJ. 180 (5): 583. doi:10.1503/cmaj.080724. ISSN 0820-3946. PMC 2645467. PMID 19255085. [View]
- Ruddy, Stephanie M.; Bergstrom, Reece; Tivakaran, Vijai S. (2019), “Roth Spots”, StatPearls, StatPearls Publishing, PMID 29494053 [View]
- Herbort CP et al. (2017). “Why birdshot retinochoroiditis should rather be called ‘HLA-A29 uveitis’?”. Br J Ophthalmol. 0 (7): 2016–309764. doi:10.1136/bjophthalmol-2016-309764. PMC 5530806. PMID 28314830. [View]
- https://www.medicinenet.com/brushfields_spots/definition.htm
- D. McLeod (September 1981). “Reappraisal of the retinal cotton-wool spot: a discussion paper”. J R Soc Med. 74 (9): 682–86. doi:10.1177/014107688107400912. PMC 1438890. PMID 6169833. [View]
YOU MAY ALSO LIKE
Rings in Eyes (Ophthalmology): Cholesterol, Blue, & More
Lines in Eyes (Ophthalmology): Arlt, Vogt, Haab’s Striae, & All

