Today’s topic is all about the macula lutea of the eye, its anatomy, function, and various problematic conditions. So, stay connected.
What is the Macula Lutea of the Eye?
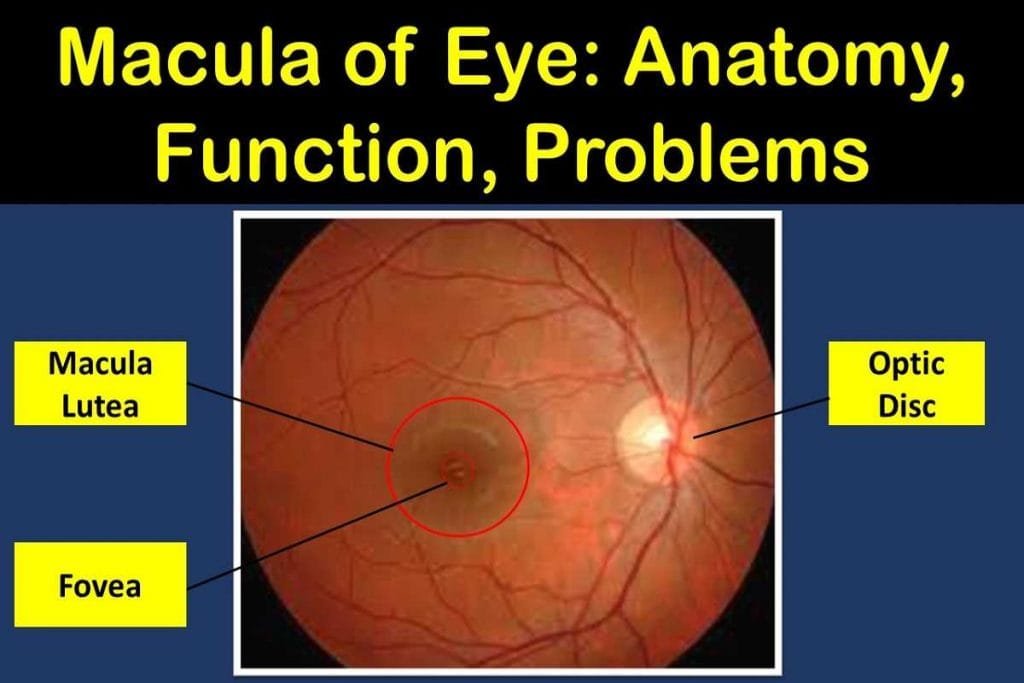
The macula lutea is an oval-shaped, pigmented, light-sensitive area near the center of the retina in the posterior pole of the eyeball. It is one of the most important parts of the eye that is responsible for our central vision or visual acuity and color perception.
The macula lutea — or just macula — has a central depression which is known as the fovea. The fovea has a high concentration of cones, which are responsible for color vision.
The photoreceptor-rich area of the retina or the macula lutea also helps us to see in dim light or at night because it contains many rods that allow us to see in low light conditions.
The macula is responsible for our ability to see fine detail, recognize faces, drive and read. Although the macula lutea is a small area of about 5.5 mm diameter in size, it gives us the ability to see “20/20”.
Anatomy of the Macula Lutea of the Eye
Color: Why is it known as Macula Lutea?
The term “Macula” is popular among the majority of the people, but it is also known as the Macula Lutea. The term “macula lutea” comes from Latin “macula,” meaning ‘spot’, and “lutea,” meaning ‘yellow’.
Unlike other areas of the retina that have red color, the macula has a yellowish appearance, which can be clearly seen in the clinical photograph, due to macular pigment, lutein, and zeaxanthin (yellow xanthophyll carotenoids) derived from your diet.
The macular pigment absorbs excess blue and ultraviolet light and protects the photoreceptor cells in the macula from the potentially harmful effects of these lights. The blue light comes from natural sources like the sun or artificial sources like computer screens.
Structure
There are two types of photoreceptor cells that can be found in the retina. These cells – called rods and cones – make our sense of sight possible by converting light rays into neural signals that are transmitted to the brain, signifying how light is seen by the eye and creating a sense of vision.
The macula contains a very high concentration of cone photoreceptor cells, which are needed for color vision as well as the ability to see fine details.
There is a very high concentration of cone photoreceptor cells in the macula, which are responsible for our color vision and our ability to see fine details.
Out of an estimated 6-7 million cone cells in the entire retina surface, almost half of them are found in the macula. The highest concentration of cones is in the fovea (or fovea centralis), which is like a pit in the macula lutea of the retina that contains only cone cells.
Macula lutea, the vital part of the retina covers an area of about 0.22 inches and can be seen with the help of an ophthalmoscope, slit lamp with fundus lens, or a fundus camera. The macula is divided into 6 clear zones-umbo, foveola, foveal avascular zone, fovea, parafovea, and perifovea.
Location
The pigmented part of the retina or macula lutea is located near the center of the retina. It is not perfectly at the center, but 1.5 mm away (towards the nasal side) from the center of the retina.
The clinical macula, which is seen through the ophthalmoscope, or retinal camera, is about 1.5 mm in size, whereas the anatomical macula, which is defined histologically (containing 2 or more layers of ganglion cells), is around 5.5 mm in diameter.
Function of the Macula Lutea
The macula at the back of the eye is important because it collects the light energy accumulated by the structures in front of it, and converts that light impulse into neural signals that go to the brain via a visual pathway where the final image formation happens.
The macula lutea is responsible for all of our sharp central vision, color vision, and process of the fine details of the objects.
Being the vital structure responsible for the central vision, diseases that affect the macula such as macular degeneration can lead to the loss of central vision.
For clear vision, it is essential for the macula, or center of the eye’s retina, to be undisturbed and relatively dry. This structure has a unique ability- one that separates humans from other beings on earth.
Clinical Significance of Macula Lutea of the Eye
Damage to the macula often results in a decline in central vision. However, since peripheral vision is left intact, those with damage can still undertake some daily activities such as walking around and driving.
The macula is the central part of the retina that controls your central vision. The most common problem with it is macular degeneration but other conditions may also affect it, e.g., edema and a hole in the middle of it.
Age-Related Macular Degeneration (ARMD)
Age-related macular degeneration (ARMD or AMD) is a condition that causes damage to the macula, a small spot in the retina at the back of your eye. It’s one of the leading causes of blindness in people over 50 and there are currently no treatments to cure it.
With AMD, your central vision starts to fade and you can’t see things in the center of your sight. But your peripheral vision stays normal. For example, imagine trying to look at a clock with hands. If you have ARMD, you’ll see only numbers of the clock but won’t see any of the hands.
There are two types of AMD: dry AMD and wet AMD
Dry Age-Related Macular Degeneration (Dry ARMD)
Around 8 in 10 people with AMD have the dry form. Dry AMD happens when the macula gets thin and the drusen start to form. You slowly lose central vision upon noticeable symptoms
There is no cure for dry AMD but it can be prevented to some extent. There are several preventive measures to choose from, like nutritional supplements or eye drops.
Wet Age-Related Macular Degeneration (Wet ARMD)
As opposed to dry AMD, wet AMD is less common but more serious. Wet AMD is when abnormal blood vessels grow beneath the retina. The vessels leak blood or other fluids and scar the macula, leading to vision loss.
Wet AMD is much more serious because it can lead to rapid vision loss as opposed to dry AMD which usually progresses slowly
It’s hard to notice that you have AMD if you don’t regularly visit an ophthalmologist. That’s why it’s important to have regular visits. Early detection can prevent the onset of any problems with your vision, including age-related macular degeneration.
Central Serous Retinopathy
Central serous retinopathy (CSR) is an eye condition that causes sudden or gradual blurry vision due to fluid buildup beneath the retina.
The retina is a layer of cells that sends signals to the brain, providing information about what we see. The cells are called photoreceptors and they are responsible for translating light into electrochemical impulses. CSR causes fluid buildup behind the retina.
If the macular area has CSR, the person starts noticing the sudden or gradual blurry and distorted vision in the affected eye.
There might be a chance that the fluid accumulation happens at the peripheral retina, not at the macular region. In such conditions, the consequences may not give you any signs that anything is wrong and it’s possible to have CSR without realizing it.
In the majority of the cases, CSR doesn’t require any treatment as the accumulated fluid drains by itself over time. In rare cases, the fluid beneath the retina should be drained with intervention such as medications, photodynamic therapy, laser treatment, among others.
Diabetic Macular Edema
Diabetic retinopathy is a complication of diabetes and can lead to a number of changes in the eye – from mild changes to severe, sight-threatening damage.
Sometimes, tiny blood vessels increase in size, rupturing and leaking fluid into the retina. This fluid can cause swelling in the central part of the retina (macula). This is a serious eye complication that can cause vision problems or blindness. It is called diabetic macular edema.
There are effective treatments available for diabetic macular edema. Annual eye exams can detect any changes early, and could help with reversing vision loss.
When you have diabetic macular edema, your doctor may prescribe more than one treatment method to protect your eyesight and give you the best quality of life possible. Laser therapy and injectable medicines are the common treatment options available for diabetic macular edema.
Macular Hole
A macular hole can be caused by a small break in the macula, the light-sensitive tissue at the center of your eye. It is responsible for sharp, central vision and seeing fine details.
A macular hole is a condition often associated with aging in which the central vision becomes blurred and distorted. This commonly occurs in those over 60 years of age
Macular holes often start gradually, in the early stage people might notice some distortion or blurriness of central vision.
Straight lines and objects can start to look distorted or bent. It gets harder to read or do other routine tasks.
Some cases of macular holes heal by themselves and require no treatment. But surgical procedures are needed in most cases of macular holes, to help improve your vision. The procedure that is used for this is called a vitrectomy.
Macular Dystrophies
Macular Dystrophies are a type of rare hereditary condition that affects the vision in the central field. The most common type is Stargardt’s disease, which can appear in childhood but may not be diagnosed for many years.
Epiretinal Membrane
Other names of the epiretinal membrane are macular pucker or cellophane maculopathy.
The epiretinal membrane is a thin sheet of fibrous tissue that attaches to the retina. Epiretinal Membranes are one of many possible causes for blurred or distorted vision.
Surgery can sometimes be required in severe cases to remove the epiretinal membrane and to restore vision.
Cherry Red Spot
A cherry-red spot is a macular finding in a number of lipid storage disorders and central retinal artery occlusion. It may be seen on examination as a small central choroidal area.
The appearance of the cherry-red spot is due to the transparency of the macula, while storage disorders cause the accumulation of storage material within the cell layers of the retina. But, the transparent macula allows the eye to visualize the red choroid below.
Macular Hypoplasia
Macular Hypoplasia or foveal hypoplasia is a very uncommon eye-related condition. It causes the tiniest, central area at the back of your retina to be underdeveloped, which affects what you can see in detail. Macular Hypoplasia is often associated with other health and vision problems, such as albinism.
There are other diseases besides albinism that can also lead to foveal hypoplasia such as aniridia, retinopathy of prematurity, and Alport Syndrome.
Photic Retinopathy
Photic retinopathy is damage to the retina of the eye. Solar exposure, laser, and arc welders can cause photic retinopathy, especially on the macula of your eye.
Photic retinopathy usually happens when you stare at the Sun, a solar eclipse, or some other bright light source.
Photic retinopathy generally disappears on its own with time but there is no medical treatment that has been found to speed up recovery. One path sometimes attempted with unknown results is the treatment of the initial macular edema with corticosteroids.
Symptoms of Macular Lutea Damage
When damage to the macula lutea occurs, it is common to notice changes in your central vision. For example, you may notice that straight lines appear wavy or that text on a computer screen is fuzzy. It’s important to mention these changes to your eye care professional as soon as possible.
- Reduced central vision: You may feel that there’s a blurry patch in your field of vision
- Image and line distortion: Images and lines may become distorted when vision is impaired and it’s easy to detect when you use the Amsler grid.
- Image size distortion: You might find objects look bigger or smaller than they should. This can lead to double vision, as your unhealthy eyes see things differently.
How to Keep Macula Lutea Healthy?
The first important way to look after the macula lutea of the eyes is routine eye exams because it really saves you from getting any nasty eye diseases like macular degeneration.
As part of a comprehensive eye exam, your optometrist or ophthalmologist can examine the health of your macula lutea through visual acuity test, macula function test, along with other tests, and identify any signs of potential damage before they have a chance to permanently affect your vision.
Another key point is to keep your eyes healthy. Dietary improvements and lifestyle choices can decrease your risk for diabetes & cardiovascular disease, both are responsible for negatively affecting macula health and deteriorating vision.
YOU MAY ALSO LIKE
Colored Part of the Eye: Iris Definition, Function, & Anatomy
What is the conjunctiva of the eye? Definition, Anatomy, Function
Vitreous Humor of the Eye: Anatomy, Function, & Problems
White Part of the Eye: Sclera Function, Definition & Anatomy
What is Cornea of Eye: Function, Definition, Anatomy, Layers

