All about bulbar conjunctiva, palpebral conjunctiva, and fornix of eye.
Bulbar Conjunctiva, Palpebral Conjunctiva, and Fornix of Eye
Conjunctiva, a fine transparent membrane that covers the white part of the eye and the inner lining of the eyelid, is broadly divided into three parts or segments. These 3 parts of the conjunctiva are palpebral conjunctiva, bulbar conjunctiva, and conjunctival fornix of eye.
We will be talking about all types of conjunctiva along with plica semilunaris, and the caruncle. So, stay with us till the end.
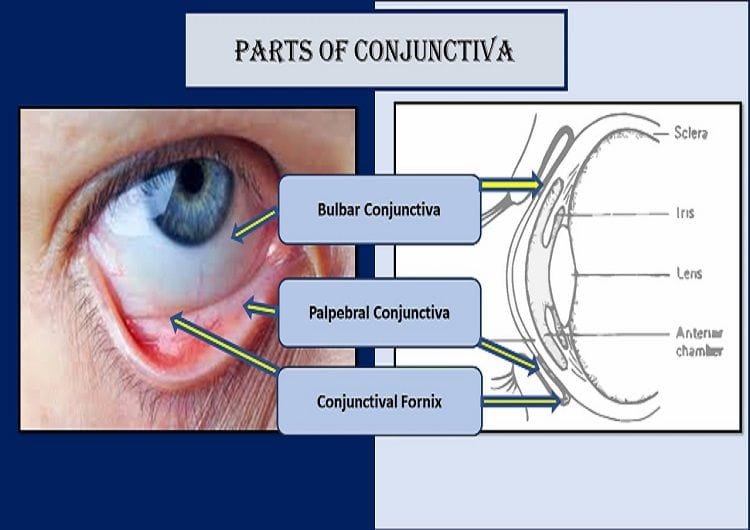
Bulbar Conjunctiva
The bulbar conjunctiva is the thinnest of all the conjunctiva. It is so translucent that the underlying white part of the eye (sclera) and blood vessels are observed vividly. Bulbar conjunctiva can be moved easily as it is loosely attached over the underlying episcleral tissues (except at the limbus and near insertions of the recti muscles). In the episcleral region lie the anterior ciliary arteries, forming a pericorneal plexus, and tendons of the recti. There are two parts of the bulbar conjunctiva: scleral conjunctiva and limbal conjunctiva.
Scleral Conjunctiva
Episcleral tissue and Tenon’s capsule (fascia bulbi) lie between the sclera and the bulbar conjunctiva. This type of conjunctiva is called scleral conjunctiva.
Limbal Conjunctiva
The part of the bulbar conjunctiva that lies at the limbal zone (3 mm near the limbus) and is densely fused with the corneal epithelium is defined as limbal conjunctiva. The less mobile limbal bulbar conjunctiva, sclera, and the Tenon’s capsule fuse together and thus helps to maintain a firm hold of the globe with forceps during ocular surgery. Hence, the limbal region has clinical significance.
The palpebral and bulbar conjunctiva form a continuous sheet between eyelid and eyeball. It means, the conjunctiva doesn’t allow any objects from the anterior region to pass towards the posterior covering of the eyeball. Thus, it reduces the risk of anything gets lost behind the eye. It is useful clinically for contact lens wearers and prosthetic eye users.
Palpebral Conjunctiva
The Palpebral conjunctiva (Palpebral Portion) is thick, opaque, highly vascular, and covered with numerous papillae, its deeper part presenting a considerable amount of lymphoid tissue. At the margins of the lids, it becomes continuous with the lining membrane of the ducts of the tarsal glands, and, through the lacrimal ducts, with the lining membrane of the lacrimal sac and nasolacrimal duct.
At the lateral angle of the upper eyelid, the ducts of the lacrimal gland open on its free surface; and at the medial angle, it forms a semilunar fold, the plica semilunaris.
The palpebral conjunctiva lines or covers the inner surface of the eyelids. Depending on the position of the eyelids, there are upper and lower palpebral conjunctiva. The palpebral conjunctiva is subdivided into 3 parts: marginal palpebral conjunctiva, tarsal palpebral conjunctiva, and orbital palpebral conjunctiva (orbital zones).
Marginal Conjunctiva
The marginal conjunctiva lies at the eyelid margin. It is a transition area between the conjunctiva sheet and the eyelid skin. The marginal palpebral conjunctiva extends from the eyelid margin to 2 millimeters on the back of the lid up to a shallow depression (or groove) known as sulcus subtarsalis (subtarsal fold). The perforating blood vessels (branches of the marginal arcade) traverse the tarsus to the conjunctiva near this groove.
The puncta (the opening of the lacrimal passage) opens in the marginal conjunctival zone. This punctal opening forms the continuous passage between the conjunctival sac and the nasal inferior meatus through the lacrimal passage. Thus, the nasal infection may spread to the eye and vice versa (conjunctival infection may spread to the nose).
Sulcus subtarsalis or subtarsal sulcus is the common site for lodgment of the conjunctival foreign body. Thus, this area is clinically significant.
Tarsal Conjunctiva
Tarsal conjunctiva is a thin, transparent, and highly vascular sheet. It intimately adheres to the tarsal plats of both upper and lower eyelids. Attachment is more marked in superior tarsus than in inferior tarsus. The tarsal conjunctiva is fully adherent to the upper eyelid while it is adherent only to half-width of the inferior tarsus.
The tarsal glands appear as parallel yellow streaks in a vertical fashion through the translucent tarsal conjunctiva.
It is almost impossible to separate the conjunctiva and tarsal plate by dissection. So, the surgical repair at this site is very difficult.
The tarsal conjunctiva is a common site for follicular and papillary reactions in conjunctivitis. Clinically, the reactive pathology of the conjunctiva due to any reason may be seen in the palpebral conjunctiva.
Orbital Conjunctiva
The orbital part of the palpebral conjunctiva is loosely placed between the fornix and the tarsal upper border. It is folded horizontally during eye movements (most when the eyes are open and least when they are shut) due to its loose attachment to the subjacent non-stratified muscle. These folds are developed after the birth of a child.
During slit lamp examination, a series of shallow grooves which create a mosaic of low elevations are seen just above the superior tarsus under low magnification. These mosaic structures are known as Stieda’s plateau and grooves (pseudo papillae).
Conjunctival Sac
Bulbar and palpebral conjunctiva and fornix form a sac in between eyelid and eyeball that opens at the palpebral fissure. The conjunctival sac has the capacity to hold fluid up to 30 µl (microliter). The sac already contains about 7 µl of tear fluid forming a tear prism.
This knowledge is helpful to answer the query regarding how many drops of medicinal eyedrop can a person put in an eye at a time. A standard eyedropper dispenses 0.05 ml (50 µl) per drop, meaning there are 20 drops per ml. Based on this calculation we can say that one drop of eyedrop is more than enough for the eye to hold. So, it is a complete waste of eyedrop if you use more than one drop at a time.
Conjunctival Fornix of eye or Forniceal Conjunctiva
Conjunctival fornix or forniceal conjunctiva is a circular cul-de-sac that joins the palpebral and bulbar conjunctiva. It is a continuous sheet that ends only on the medial or nasal side by the caruncle and the plica semilunaris. The conjunctival fornix is comparatively thicker and loosely adhered to allow free eyeball movement. Forniceal conjunctiva can be subdivided into superior, medial, inferior, and lateral fornix of the eye.
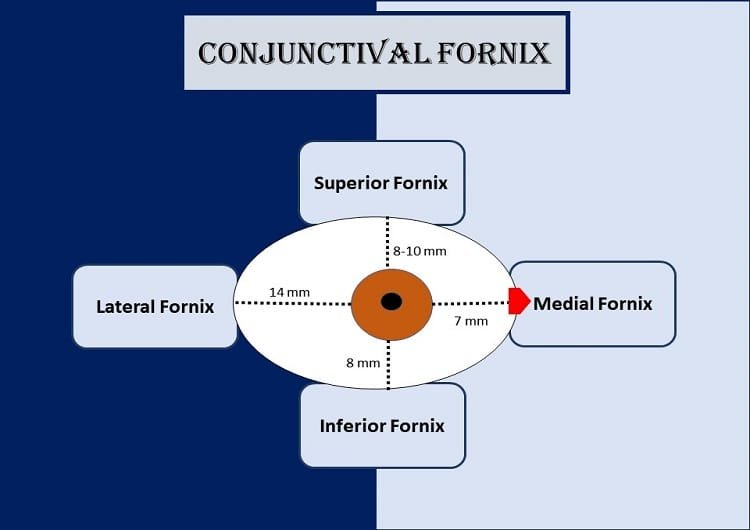
Superior fornix
The superior fornix or superior conjunctival fornix lies between the eye globe and the upper eyelid. It extends from the upper border of the tarsus to 8-10 mm above the upper limbus, and reaches a superior orbital margin. It gets attached superiorly to the fascial sheath of the superior rectus muscle and the levator palpebrae muscle. Any foreign body in the superior fornix can be removed by the double eversion of the eyelid.
Inferior fornix
The inferior fornix or inferior conjunctival fornix lies between the eye globe and the lower eyelid. It lies within few millimeters of the inferior orbital margin to 8 mm below the lower limbus.
Medial fornix
The medial fornical conjunctiva is the most shallow, comprising medial ends of the inferior and superior fornices. The 7 mm conjunctiva contains the caruncle and the plica semilunaris at the nasal most part.
Lateral fornix
The lateral forniceal conjunctiva lies between the eyeball and the lateral canthus. It extends up to a distance of 14 mm from the lateral temporal or lateral part of the limbus.
Plica Semilunaris
The plica semilunaris is a narrow crescentic fold of conjunctival fornix, concave laterally, and present in the medial canthus lying lateral to and partly behind the caruncle. It is a vestigial structure in human beings. Plica semilunaris represents the nictitating membrane of the lower animals.
The plica reaches the middle of the lower fornix below and extends less far above. 2 mm recess separates the free lateral border from the bulbar conjunctiva, and it disappears in the lateral gaze of the eyeball. Its vascular, pink color contrasts with the white part of the eye, the sclera.
Numerous goblet cells are present in plica semilunaris that may be superficial or grouped with a narrow duct. Melanophores are always present and may be non-pigmented in blonde persons.
The connective tissue stroma in the plica is vascular, loose, and contains a nodule of fibrocartilage.
Caruncle
The caruncle (Latin caro=flesh) is a small, soft, pinkish mass in the inner or nasal canthus medial to the plica semilunaris. It is a piece of modified skin and has sweat glands, hair follicles, and sebaceous glands.
The caruncle is about 5 mm high and 3 mm broad. It adheres to the plica semilunaris, and fibers of the medial rectus sheath. Hence, the caruncle is prominently visible in lateral gaze and becomes retracted on the medial gaze of the eyeball.
The caruncle contains goblet cells, lacrimal tissue, hairs, medially directed sebaceous glands, and sweat glands. The epithelium is composed of non-keratinized, stratified squamous cells.
The superior medial palpebral arteries supply blood to the caruncle. The lymphatic drains into the submandibular lymph nodes. similarly, the infratrochlear nerve innervates the caruncle.
Blood Supply to the Bulbar Conjunctiva, Palpebral Conjunctiva, and Fornix
Anterior conjunctival arteries and posterior conjunctival arteries supply blood to the bulbar conjunctiva. Similarly, conjunctival fornices of the eye and palpebral conjunctiva get blood supply from the arterial branches from the marginal and peripheral arcade of eyelids.
The posterior conjunctival arteries are the branches of the arterial arcades of the eyelids and the anterior conjunctival arteries derive from the anterior ciliary arteries. The anastomosis of two types of arteries gives rise to pericorneal plexus.
The veins around the cornea drain blood from the bulbar conjunctiva in the limbal region into the anterior ciliary veins and veins from the remaining parts of the conjunctiva drain blood into the venous plexus of the eyelids, and ultimately to the superior and inferior ophthalmic veins.
Lymphatic Drainage of the Bulbar Conjunctiva, Palpebral Conjunctiva, and Fornix of Eye
Lymphatics of underlying eyelids, submandibular, and preauricular lymph nodes are responsible for the lymphatic drainage of the palpebral, bulbar conjunctiva, and forniceal conjunctiva. Lymphatics of the palpebral conjunctiva drain into the lymphatics of eyelids. Likewise, nasal bulbar conjunctival lymphatics drain into the submandibular lymph nodes, and the temporal bulbar conjunctival lymphatics drain into the preauricular lymph nodes.
Nerve Supply
The superior palpebral conjunctiva is innervated by the supraorbital, supratrochlear, infratrochlear, and lacrimal nerves whereas the inferior palpebral conjunctiva is supplied by the lacrimal and infraorbital nerves.
The superior fornix is innervated by the supraorbital, supratrochlear, infratrochlear, and lacrimal nerves while the inferior fornix is supplied by the lacrimal and infraorbital nerves. The ciliary nerves innervate the bulbar conjunctiva.
YOU MAY ALSO LIKE
Blurry Vision In The Morning – Causes And Concerns
Colored Part of the Eye: Iris Definition, Function, & Anatomy
Wavy Squiggly Lines in Vision (Eye Floaters)
What is Conjunctiva of the Eye?
White Part of the Eye: Sclera Function, Definition & Anatomy
What is Cornea of Eye: Function, Definition, Anatomy, Layers
Optic Nerve: Definition, Function & Anatomy
References
- Wolff’s Anatomy of the Eye and Orbit by Anthony J. Bron, Ramesh C. Tripathi, Brenda J. Tripathi
- Comprehensive Ophthalmology Fourth Edition by A. K. Khurana