Corneal collagen cross-linking eye surgery is the new treatment for people with keratoconus. When nothing else was able to stop this corneal disease from getting worse, cross-linking eye surgery provides hope for patients with keratoconus.
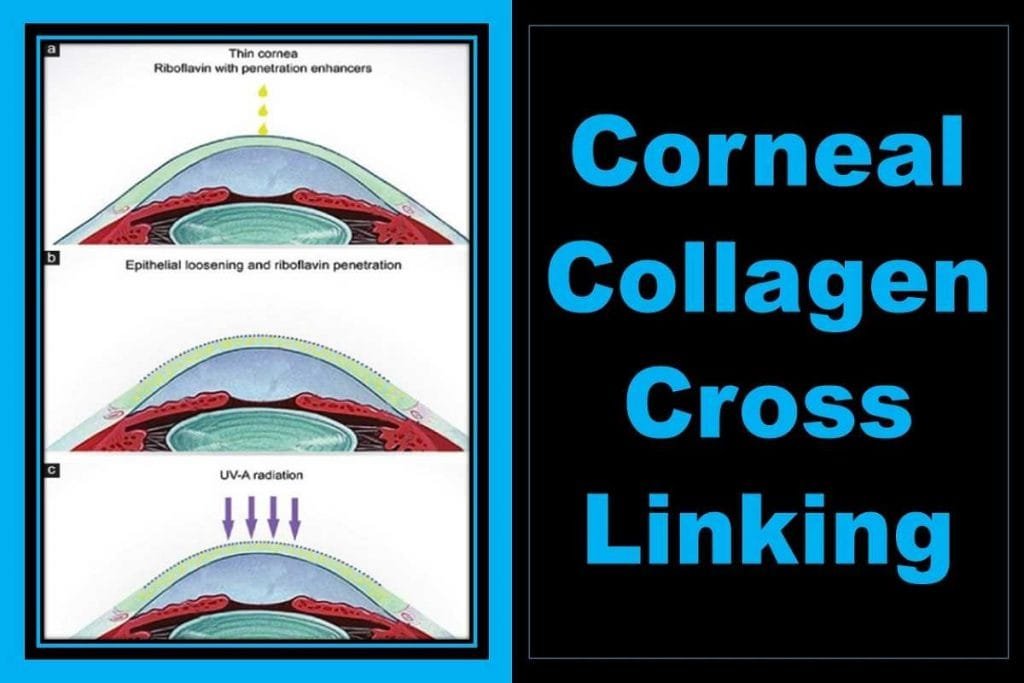
Corneal collagen cross-linking is a surgical procedure that strengthens the cornea. The process involves inserting riboflavin drops into the eye and then exposing it to ultraviolet light. This treatment will strengthen the cornea and reduce or eliminate keratoconus and other corneal ectatic conditions.
Cross-linking eye surgery is becoming a more popular treatment for stopping the progression of corneal diseases. Read on to learn about everything that this procedure entails.
Corneal cross-linking is a quick and easy outpatient procedure that usually lasts for about an hour.
This is a new procedure, as it was only approved by the FDA in 2016 for use in the United States, although it was used in other countries before.
What is Corneal Collagen Cross-linking?
Corneal collagen crosslinking (CL or CXL) is a simple and minimally invasive procedure that can help prevent the progression of certain eye conditions such as keratoconus and post-LASIK ectasia. Cross-linking is a treatment that improves the strength of your cornea.
In a corneal cross-linking procedure, your doctor will apply riboflavin (vitamin B2) eye drops to the surface of your eyes before shining an ultraviolet light to strengthen them.
The liquid used in eye drops contains the molecular substance that participates in a photoreaction (a series of chemical reactions) with another molecule. The procedure causes new corneal collagen cross-links to develop. They cause the collagen fibrils to shorten and thicken, which makes your cornea healthier and stronger.
Types of Corneal Collagen Cross Linking
Two corneal cross-linking types include:
Epithelium-off cross-linking.
With this cross-linking procedure, the corneal outer layer or epithelium is removed to allow for more deep tissue to be penetrated by the vitamin riboflavin liquid.
Epithelium-on cross-linking.
This cross-linking procedure is considered a less invasive corneal procedure than cross-linking with the removal of the corneal epithelium. The protective corneal epithelium is left intact during this procedure.
Different strategies have been tried to avoid some of the irritation and discomfort of epithelium removal. This includes the use of pharmacological agents to loosen the intraepithelial junctions, the creation of intrastromal pockets for direct introduction of riboflavin, and iontophoresis.
Epithelium-on cross-linking may be able to avoid complications, like postoperative pain and corneal haze, but research suggests it’s less effective than epithelium-off cross-linking.
Currently, the only US FDA-approved method for treating progressive keratoconus is epithelium-off crosslinking done with Glaukos KXL System and proprietary Photrexa and Photrexa Viscous solutions.
Any drug other than Photrexa and Photrexa Viscous or any device other than the KXL System for corneal cross-linking is not FDA approved, with the exception of investigational new drugs
Glaukos has been able to make a safe and efficient corneal cross-linking procedure. The Phase 3 trial was a success and should be completed soon!
Alternative to Corneal Collagen Cross-Linking
For many years, people suffering from Keratoconus had no options when it came to treatments. Now there is a breakthrough procedure to combat this debilitating condition.
Currently, there are few treatment options available (surgical and non-surgical) for those with keratoconus, like specialty contact lenses, intacs. However, corneal cross-linking is the only treatment that has been proven to improve vision in those with progressive keratoconus, without using eyeglasses or contact lenses.
Keratoconus Treatment in the Past and Now
Keratoconus is an eye disorder in which a person’s cornea starts to bulge away from the eye, causing a cone-like shape. These underlying changes in the cornea can make it difficult to see and lead to distorted vision.
Keratoconus usually develops during the teenage years, but the thinning tends to get progressively worse for about 10-20 years. It’s possible for the rate of progression to change over an individual’s lifetime, but most cases have their worst phase during adolescence and eventually stabilize by adulthood.
Before the US Food and Drug Administration approved cross-linking in 2016, keratoconus was treated with glasses, contacts, and surgical implants or Intacs®.
These treatments help correct vision changes but they don’t have a notable effect on progressive corneal thinning.
As a result, many patients with keratoconus, unfortunately, needed to wait for their condition to progress and worsen before they knew whether they will need a cornea transplant.
All that worse time has changed, the procedure for corneal cross-linking can be done on teens and it stops the thinning of your corneas.
Candidates and Criteria for Corneal Collagen cross Linking
Keratoconus is a common eye condition, and many people find that the corneal collagen cross-linking procedure is helpful. It can be used on those with this issue from birth or from an event like another surgery. Sometimes it doesn’t work for everyone though, so we advise discussing this fully with an eye doctor beforehand.
If you have post-operative keratoconus (which developed after surgery), cross-linking may help to reverse the damage and restore the shape of your cornea.
If you have the genetic or hereditary form of the keratoconus, then the answer is a little bit more complicated
Hereditary keratoconus is progressive and often worsens earlier in life. But, as you get older, you may reach a stable level of the disease. Your eyes and vision may not get better but the shape of your corneas will remain unchanged.
Research shows cross-linking is recommended only in the case of progressive keratoconus. If your eye and visual status have not changed each year, surgery is not recommended.
The American Academy of Ophthalmology warns that corneal collagen cross-linking surgery is not right for people with:
- Patients with less than 400 microns of cornea thickness cannot be treated with the standard treatment protocol of corneal cross linking
- If you have been previously infected with herpes virus, it is advisable to avoid procedures as it would trigger a viral reactivation. Similarly, the eyes with recurring infection and active infection of any type are contraindicated for corneal cross linking.
- If your cornea has scars or previous injuries or infections, you might have the potential for more eye problems.
- You cannot get corneal cross-linking surgery if you have a history of wound healing problems, like a poor epithelial wound-healing record.
- For anyone with a problem of severe dry eyes or other ocular surface disease, corneal cross-linking surgery is not a good choice.
- Sufferers of autoimmune diseases have a poorer prognosis for healing and this is true for their eyes, too. This means that an eye doctor will advise you not to go for corneal cross-linking surgery if you are suffering from an auto-immune disease.
Corneal Cross-Linking Procedure
Before the Surgery
Prior to the surgery, your eye doctor will measure the thickness of your cornea and confirm you are a good candidate for corneal cross-linking surgery. You will also need to have an eye exam to check your general eye health and vision.
Your eye doctor will also perform the corneal topography test to map the shape of your cornea.
On the Surgery Day
On the day of your cross-linking procedure, don’t wear eye makeup, perfume, or aftershave. You’ll be able to have a light meal and drink fluids
You’ll need someone to drive you home after your procedure for your safety and well-being.
You should follow the instructions from your eye care provider.
One of the great things about a cross-linking procedure is that you can go home on the same day.
You can expect the following activities during the corneal collagen cross-linking surgery.
The first thing that will be done is to numb your eye by injecting a numbing eye drop.
Your eye doctor will remove the thin epithelial layer from your cornea. This will allow the medication to get deeper into your cornea and numb it more effectively. Don’t worry about feeling pain, because all those numbing drops should help soothe the discomfort during the procedure.
Then, vitamin B (riboflavin) eye drop medicine will be installed on the cornea for about 30 minutes.
Now, a specialized device will shine a UV light at your eye for 30 minutes. This process activates the vitamin B in your cornea to assists the process of forming new bonds between the collagen fibers in the cornea of your eye.
After the Surgery
Once you’ve had corneal collagen cross-linking procedure, here’s how to take care of your eyes:
You may experience mild discomfort for up to a few days after your surgery, however, your eye doctor will provide you with medication if necessary.
Bandage contact lenses are placed over the eyes and left in place for about a week. They help your cornea heal faster, and minimize pain in your eyes. Your eye doctor will prescribe you to put antibiotic and steroid eye drops to help heal the eyes.
Be careful not to rub your eyes for 5 days after cross-linking surgery.
You may have increased light sensitivity. Sunglasses may help. You might feel like something is in your eye at first.
If you start experiencing severe pain or a sudden worsening of your vision then you should visit the doctor.
Risk of Corneal Cross-Linking
Like all surgical procedures, corneal cross-linking involves some risk.
While corneal cross-linking does involve removing the thin layer at the surface of your cornea (corneal epithelium), it can carry substantial risks such as corneal epithelial haze, epithelial defect, and slow epithelial healing process.
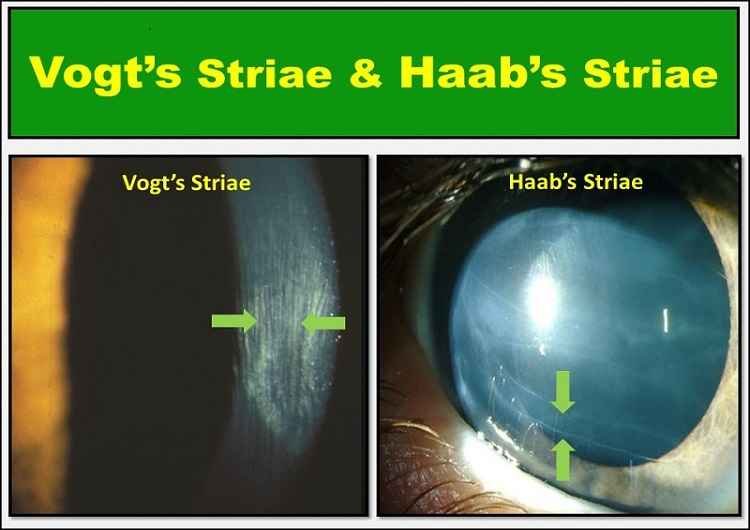
Other potential risks of corneal collagen cross-linking may include infectious keratitis, herpetic keratitis, corneal opacity, blurry vision, stromal scarring or corneal striae, ulcerative keratitis, and blurry vision.
Corneal cross-linking has a low-risk profile. Talk to your eye doctor about side effects if you’re considering this treatment.
How Much is the Cost of Corneal Collagen Cross-Linking?
The price of corneal cross-linking in the USA varies between 2,500 USD and 4,000 USD
Insurance coverage for the FDA-approved epithelium-off cross-linking procedure with Photrexa drug formulations and the KXL system from Glaukos is available to most people.
In order to understand what you’re looking at and all your options, it’s important to ask your eye doctor or insurance company. You’ll be able to find out more about the cost of the procedure and make a better decision because of it.