All About Glaucoma in Eye: Definition, Prevalence, Types, Symptoms, Causes, Prevention, Diagnosis, Treatment, and Risk Factors.
What is glaucoma in eye?
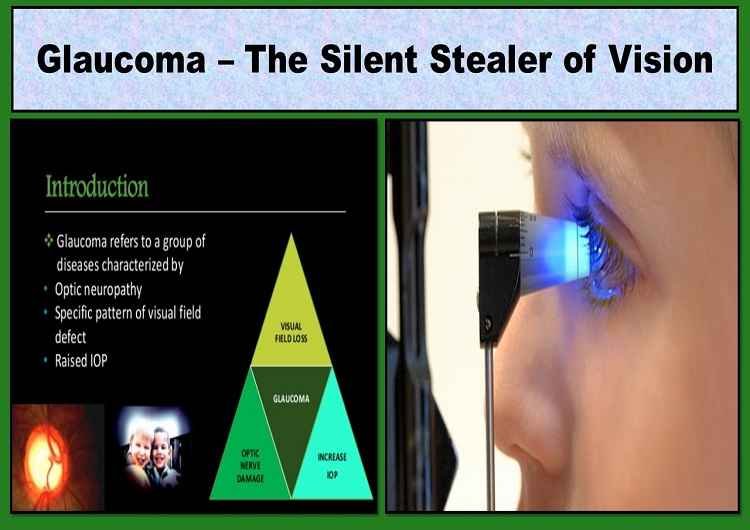
Glaucoma in the eye may be defined as a group of diseases characterized by a triad of optic neuropathy, raised intraocular pressure (IOP), and a specific pattern of visual field defect.
In glaucoma, the optic nerve of the eye is damaged, which leads to irreversible blindness. This is usually due to high IOP inside the eyes.
The optic nerve is a bundle of nerve fibers connecting the retina to the brain. When the optic nerve is damaged, the visual signals (that tell your brain what you are seeing) are interrupted.
If this pressure on the optic nerve and other parts of the eye is not controlled, then the person can become blind forever. Glaucoma is one of the major causes of blindness in the world. It can occur at any age but is more common in older people.
Initially, there are no symptoms of glaucoma. Its effect is very slow and insidious. The person with secondary glaucoma does not see or feel any symptoms until there is irreversible damage to the optic nerve and loss of a large portion of the peripheral visual fields. That’s why glaucoma in eye is also known as ‘The Silent Stealer of Vision’.
The lost eyesight due to glaucoma cannot be regained again. Therefore, it is important to get your eyes (and intraocular pressure) checked regularly. If glaucoma is identified early, vision can be prevented from getting worse.
Your doctor needs to pay more attention to correctly diagnose glaucoma. He will check the pressure on your eyes on a regular basis to find out if you have glaucoma. If you have this disease, then you may need treatment for your whole life.
There are different types of glaucoma. These may include open-angle, angle-closure, normal tension, pigmentary, congenital, and secondary glaucoma. The most common among these is open-angle glaucoma.
How common is glaucoma in eye? (Global Prevalence of Glaucoma)
Glaucoma is a common eye disease. It can occur at any age but, it is more likely in people over 60 years of age. This is one of the major causes of blindness. According to the American Academy of Ophthalmology (AAO), the global prevalence of glaucoma for the population aged 40–80 years is 3.54%.
According to AAO, the prevalence of Primary Open Angle Glaucoma (POAG) is highest in Africa (4.20%), and the prevalence of Primary Angle Closure Glaucoma (PACG) is highest in Asia (1.09%).
In 2013, the number of people (aged 40–80 years) with glaucoma worldwide was estimated to be 64.3 million, increasing to 76.0 million in 2020 and 111.8 million in 2040.
Types of Glaucoma in Eye
There are mainly five types of glaucoma which are mentioned below:
- Primary Open-Angle Glaucoma
Primary (or chronic) open-angle glaucoma is the most common form of glaucoma affecting the vast majority of people. In open-angle glaucoma, the anterior chamber (AC) angle is wide open for the normal flow of aqueous humor but the persistent increase in IOP damages the nerve fibers.
- Acute Angle-Closure Glaucoma
This type of glaucoma is also called acute glaucoma or narrow-angle glaucoma. It is very different from open-angle glaucoma because it increases pressure on the eyes very quickly. This happens when the tubes that drain the eye fluid are closed.
If the flow of your aqueous humor fluid is suddenly blocked, the rapid buildup of fluid can cause a severe, rapid, and painful increase in pressure.
- Normal-Tension Glaucoma
Normal-tension glaucoma-NTG is also known as low tension or normal-pressure glaucoma. This particular glaucoma damages the optic nerve fibers without any increment in IOP.
- Secondary Glaucoma
Secondary glaucoma can be caused by any disease that increases pressure on the eyes. As a result, the optic nerve is damaged and the eyesight goes out.
The effect of secondary glaucoma may be mild or severe. Treatment depends on whether it is secondary open-angle glaucoma or secondary angle-closure glaucoma.
Basically, there are four types of secondary glaucoma as given below:
Pigmentary Glaucoma
Pigment granules are present behind the iris (the colored part of the eye). These particles break down inside the eye and flow towards the tubes which drain the eye fluid and close it slowly. This causes increased pressure inside the eyes.
Pseudoexfoliative Glaucoma
This is when a crusted dandruff forms from the top layer of the lens inside the eye. This substance accumulates in the angle between the cornea and the iris (AC). This blocks the fluid drainage system of the eye and starts increasing pressure inside the eyes.
Traumatic Glaucoma
The main reason for traumatic glaucoma is an eye injury. It can result from both closed globe injury, or open globe injury. Traumatic glaucoma may occur immediately after an injury or even years later.
Neovascular Glaucoma
Neovascular glaucoma is a consequence of the abnormally formed new blood vessels above the iris and the drainage system of the eye. Neovascular glaucoma is always associated with other problems, especially diabetes. This never happens on its own.
- Congenital Glaucoma
Congenital glaucoma occurs due to malformation of the aqueous drainage system either due to hereditary defects or abnormal development during pregnancy.
Stages of Glaucoma in Eye
Glaucoma has three stages:
- Initial Phase (Mild)
There are usually no changes in vision in the early stage of glaucoma. In this stage, the high pressure may not damage the optic nerve, and hence the visual acuity and visual field are normal. The treatment goal at this stage is to reduce eye pressure with anti-glaucoma drops.
- Medium phase (Moderate)
In the middle stage of glaucoma, the optic nerve damage is sufficient enough to constrict the visual field and reduce peripheral vision. However, it is a very slow process, so people are not able to notice this change in vision and visual field.
- Late phase (Severe)
In the late stage of glaucoma, the visual field is severely reduced to tunnel vision (the only central visual field is remaining). Some people fall prey to blindness. Even in the late stages of glaucoma, eye doctors recommend eye drops. However, in some circumstances, they recommend surgery to reduce intraocular pressure.
Glaucoma Symptoms
The symptoms of glaucoma depend on its type, which is:
- Open-angle glaucoma
No symptoms are seen in the onset of open-angle glaucoma. As the disease progresses, blind spots develop in the peripheral (side) visual field Most individuals with open-angle glaucoma do not feel any change in their vision until this glaucoma severely damages the eyes.
- Angle-closure glaucoma
The symptoms of angle-closure glaucoma are sudden onset. The following are the symptoms of angle-closure glaucoma.
- Severe pain in and around the eyes
- Eye congestion
- Blurry vision
- Colored halos around the lights
- Headache
- Nausea
- Vomiting
- Normal-tension glaucoma
The pressure in the eyes of people suffering from normal-tension glaucoma is within the normal range. Here, optic nerve damage and blind spots in visual fields are seen.
What are the causes of glaucoma?
Glaucoma is the result of damage to the optic nerve. This causes blind spots to form in the visual field. This nerve damage is usually related to increased pressure inside the eyes.
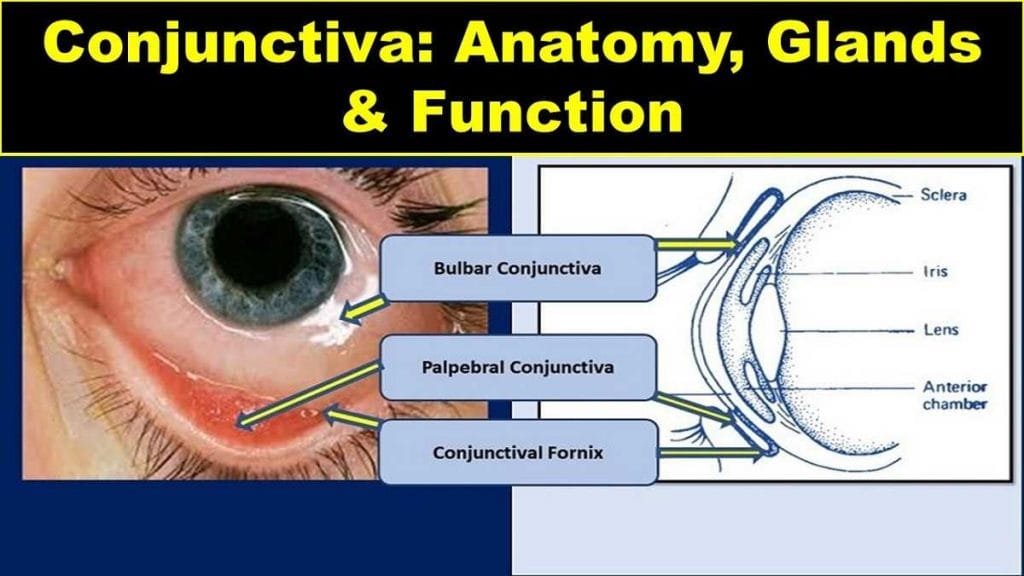
The eye pressure is caused by the formation of aqueous humor, which comes out of the eyes continuously. This aqueous humor usually collects at an angle between the iris and the cornea (AC angle).
When the aqueous is high in quantity or the drainage system does not function properly, the fluid does not flow out normally and the pressure starts to rise.
Glaucoma can spread from one member of the family to another. In some people, scientists have identified genes related to increased eye pressure and optic nerve damage.
Risk Factors of Glaucoma
There are several factors that pose the risk of glaucoma which are mentioned below
- Old age
- Some diseases, such as diabetes (sugar) or hypothyroidism.
- Eye injuries
- Eye surgery
- High myopia
- Mydriatic eyedrops
- Blocked or restricted aqueous drainage system
- Medications such as corticosteroids
Patients taking corticosteroids for a long time are at increased risk for a range of problems including glaucoma
- Decreased blood flow to the optic nerve
- High blood pressure
Prevention of Glaucoma
The devastating effect of glaucoma can be avoided by having the eyes tested regularly. The complete cure for this eye disease is not known yet. But the timely diagnosis of glaucoma helps to prevent further damage.
If the disease is detected early, blindness from glaucoma can be prevented. In the initial stage, its identification and long-term treatment maintain the vision of most people.
In general, a glaucoma checkup should be done on the following basis:
- Before the age of 40 – Every 2 to 4 years
- From 40 to 54 years of age – Every 1 to 3 years
- From age 55 to 64 – every 1 to 2 years
- After the age of 65 – every 6 to 12 months
Those who are at high risk of getting glaucoma should undergo a test every one or two years after the age of 35 to avoid it.
Your eye doctors recommend regular exercise and a nutritious diet to improve your lifestyle if you are at high risk of developing the disease. You should also take care of yourself physically, mentally, and emotionally.
Here are some points to keep in mind.
- Regular eye screening – Glaucoma can be identified and treated early by having regular eye exams.
- Exercising daily – Exercising daily is beneficial for the health and at the same time, it reduces intraocular pressure (IOP).
- Eye protection – Injuries to the eyes increase the risk of traumatic glaucoma or secondary glaucoma. Therefore, the disease can be prevented by protecting the eyes from these injuries.
- Use of eye drops – Apply the eye drops regularly as prescribed by the eye doctor.
- Knowledge of hereditary disease – Know your family’s eye health history.
Diagnosis of Glaucoma in Eye
The eye doctor will thoroughly examine your eye to diagnose the disease They will check for damage to your eye’s nerve tissue, as well as other symptoms.
Detailed Medical History
The doctor would like to know from you what kind of symptoms you are experiencing and whether your family has ever had any relationship with this problem before. They will also ask you to do a general health assessment if you have any diseases like diabetes (sugar) or high blood pressure, which can affect your eyes.
They can use one or more of the following tests and procedures.
Tonometry (IOP Measurement)
Tonometry measures the pressure within your eyes. Eyedrops are used to numb the eyes during tonometry. The physician or technician then uses an instrument called the tonometer to measure the internal pressure of the eye. Little pressure is applied to the eye by a small device or by a slight stroke of hot air.
Ophthalmoscopy (Posterior Eye Examination)
This procedure helps the doctor to check for optic nerve damage during glaucoma. Eyedrops are used to dilate the pupil of the eye so that physicians can properly examine the size and color of the optic nerve.
Perimetry (Visual Field Test)
Perimetry is a visual field test that makes a complete map of your field of vision. This test will help the doctor determine whether your vision is affected by glaucoma or not.
During this test, you will be asked to look right in front of you and be prompted when a moving light passes through your peripheral (or side) vision. This test helps to map your entire field of vision, both central and peripheral.
Gonioscopy (Examination of Anterior Chamber Angle)
This diagnostic test helps to determine whether the angle between the cornea and iris is wide open, narrow, or closed. Eyedrops are used to numb the eyes during the test.
The contact lens is gently held in the eye by holding it. This contact lens has a mirror that shows the doctor that the angle between the iris and the cornea is closed and blocked (closed angles are an indication of angle-closure or acute glaucoma) or wide and open (open-angle glaucoma or normal)
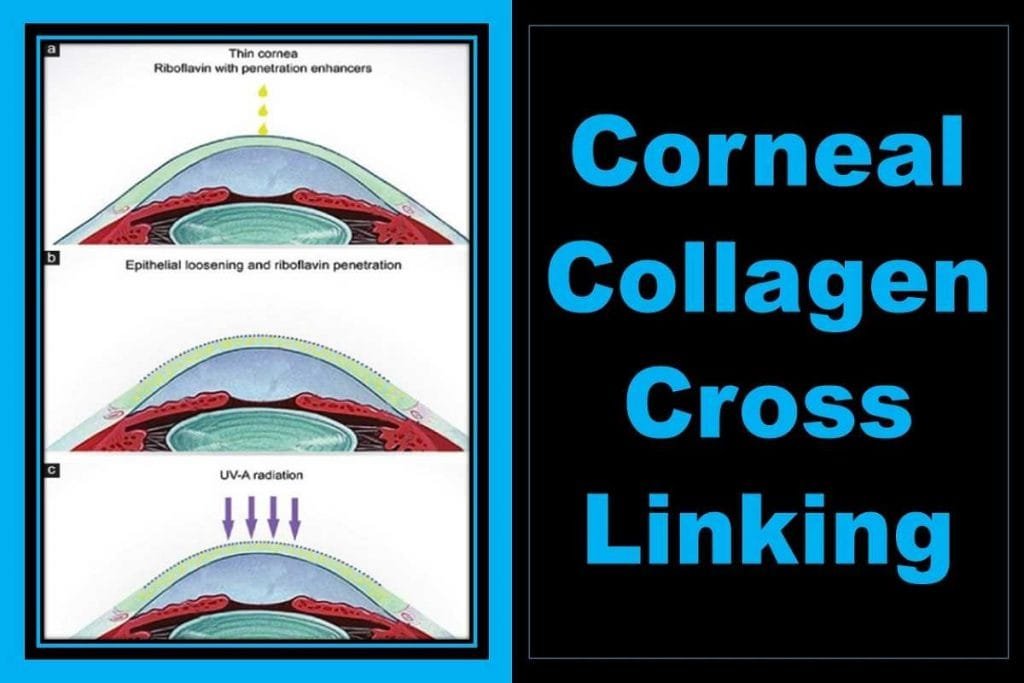
Pachymetry (Measurement of Corneal thickness)
Pachymetry is a simple and painless test to measure the thickness of your cornea. During this test, a small probe is gently placed in front of it to measure the thickness of the cornea.
A pachymetry test can aid in the diagnosis of glaucoma because corneal thickness has the potential to affect eye pressure readings. By this measurement, your doctor can understand your IOP readings better and treat you well. It takes a few minutes to measure both eyes through this process.
Treatment of Glaucoma in eye
The damage caused by glaucoma cannot be reversed or cured. If it is identified at an early stage, regular screening and treatment can reduce or prevent loss of vision.
The goal of glaucoma treatment is to reduce intraocular pressure. Depending on your situation, two treatment options are available – eye drops or surgery (laser treatment).
- Eyedrops
The first choice of treatment of glaucoma is eyedrop. The eyedrops improve the eye’s fluid drainage system or reduce the amount of fluid produced by the eyes. This reduces the pressure on the eyes. The most commonly used anti-glaucoma eye drops are:
Prostaglandins
The eye drops increase the drainage of the aqueous, which reduces the pressure in the eyes. Examples include latanoprost (Xalatan) and bimatoprost (Lumigan).
Beta-Blockers
This reduces the amount of fluid produced in the eyes, which also reduces the pressure on the eyes. These include timolol (Betimol, Timoptic) and betaxolol (Betoptic).
Alpha-adrenergic agonists
These reduce the production of aqueous humor and increase the flow of fluid through the eye. Examples include apraclonidine (iopidine) and brimonidine (Alphagan).
Carbonic Anhydrase Inhibitors
These drugs are rarely used for glaucoma. They reduce the production of fluid in your eyes. Examples include dorzolamide (Truspot) and brinzolamide (Azopt).
- Oral Medications
If the eye pressure is not brought to the desired level by instilling eye drops, your doctor may also recommend oral medicines, usually carbonic anhydrase inhibitors.
Read more about Anti-Glaucoma Eyedrops
- Surgery and other treatments
If the drainage system of the eye is closed, eye doctors may suggest surgery and other treatments to create a drainage tract for fluid or to destroy excess fluid-forming tissue. There are many types of surgeries that your doctor can recommend.
- Laser Therapy
- Filtration surgery
- Drainage tubes
- Electrocautery
But there is a different treatment for angle-closure glaucoma. This type of glaucoma requires immediate treatment as soon as possible to reduce eye pressure. A laser procedure called Laser Peripheral Iridotomy can also be performed.
Glaucoma in Eye Risks & Complications
The risk factors for glaucoma depend on the types.
1) Risk factors for Open-Angle Glaucoma
- Increased IOP
- Family history of glaucoma
- Increased age
- Thin cornea
- Increased cup-disk ratio (CDR)
- High myopia
- Diabetes
- Eye surgery or injury
- High blood pressure
- Use of corticosteroids (eye drops, tablets, inhalers, and creams)
2) Risk factors for Angle-Closure Glaucoma
- 40 years of age or older
- Family history of glaucoma
- Hypermetropia
- Eye injury or eye surgery
3) Risk factors for Normal-Tension Glaucoma
- Cardiovascular diseases
- Family history
- Ocular hypotension
What to avoid during Glaucoma in eye?
Some precautions to be taken in glaucoma not to do the following activities.
1) Caffeine Consumption
Drink coffee in moderation. Excessive consumption of caffeinated coffee is not appropriate for a glaucoma patient.
2) smoking
Smoking has been found to be related to the risk of causing glaucoma.
3) Blowing instruments
Blowing instruments are found to increase intraorbital pressure. The intraocular pressure can double within about 20 seconds while the instruments are blown but quickly return to the baseline.
4) High blood pressure
Untreated systemic hypertension is associated with glaucoma. These two are connected indirectly. The optic nerve is damaged along with blood vessels, possibly due to high blood pressure.
Therefore, it is advised that high blood pressure be treated.
5) Yoga
Yoga done in the reverse position increases the intraocular pressure in some people, which can worsen the condition of glaucoma.
6) High body mass index (BMI) and obesity
Overweight (obesity) is associated with high IOP. A high BMI (body mass index) is associated with sleep apnoea.
7) Sleep Apnoea
Sleep apnea syndrome (SAS) is associated with glaucoma. It interrupts breathing repeatedly during sleep. Patients get chronic fatigue and loss of consciousness due to sleep apnea. It is more dangerous for men who are obese, and who snore, drink heavily, and smoke.
8) Drinking Excessive Water
Drinking excessive amounts of water (500 mL to 1 liter) over a short time period (15 minutes) can cause a significant increase in IOP. Glaucoma patients should avoid consuming excessive amounts of fluids.
9) Alcohol
Alcohol may initially reduce IOP), but daily alcohol intake may cause a slight increase in IOP. Therefore, eye doctors recommend not drinking excessive alcohol.
What to eat in Glaucoma?
Regularly consume the following nutritious diet when you have glaucoma.
1) Dark green, yellow, and orange fruits and vegetables
These foods contain carotenoids, which can protect against many serious diseases including glaucoma. Lutein and zeaxanthin are particularly important for eyesight.
2) Vitamin C rich fruits and vegetables
These foods include green chilies, citrus fruits, tomatoes, broccoli, strawberries, sweets, white potatoes, and leafy vegetables.
3) Vitamin E rich foods
These include eggs, fruits, wheat, green leafy vegetables, nuts, walnut oil, vegetable oil, and whole grains.
4) Vitamin A rich foods
Liver, sweet potatoes, carrots, mangoes, milk, eggs, and barley are rich in vitamin A.
5) Foods rich in Vitamin D
Fish oil, cod liver oil, milk rich in vitamins and grains, eggs, and barley are the major sources of vitamin D.
6) Zinc-rich food
These include red meat, poultry, beans, nuts, some seafood, whole grains, nutritious breakfast cereals, and dairy products like vitamins.
7) Foods containing omega-3 fatty acids
Salmon fish, sardines, walnuts, and flax oil are good sources of omega-3 fatty acids.
Anti-Glaucoma Eye Drops or Medications PPT
Sources
- https://www.aaojournal.org/article/S0161-6420(14)00433-3/abstract
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5228680/
- https://www.nlm.nih.gov/medlineplus/ency/article/001620.htm.
- who.int/bulletin/volumes/82/11/feature1104/en/
- https://www.medicalnewstoday.com/articles/9710.php
YOU MAY ALSO LIKE Diplopia Charting: Common Method of Double Vision Test